-
PDF
- Split View
-
Views
-
Cite
Cite
Daniel Kakish, Marwan Alaoudi, Brian Welch, David Fan, Melissa Meghpara, Nageswara Mandava, Narendra Kumthekar, Small bowel intussusception in marijuana users, Journal of Surgical Case Reports, Volume 2020, Issue 9, September 2020, rjaa335, https://doi.org/10.1093/jscr/rjaa335
Close - Share Icon Share
Abstract
Intussusception occurs when one portion of bowel ‘telescopes’ into another due to a lead point created by a range of benign or pathologic process. Intussusception mostly occurs in children. Although adult intussusception (AI) is rare, accounting for <5% of intestinal obstructions, it is more concerning in adults as malignancy accounts for nearly 65% of lead points in AI. Patients present with severe abdominal pain concerning for an acute abdomen along with a degree of bowel obstruction. We have experienced a total of 11 patients within recent years presenting with symptoms of an acute abdomen due to AI. None of these patients were found to have a pathologic process creating a lead point. However, we found that all of them were marijuana users. In this report, we compare their management, hospital course and review of the literature discussing proposed mechanisms that suggest an association between cannabis and intussusception.
INTRODUCTION
According to the National Institute on Drug Abuse, in 2013 there was an estimated 24.6 million Americans who have reported illicit drug use at some time. Marijuana was the most commonly used illicit drug, making up 19.8 million users, an increase from the 14.5 million users reported in 2007 [1]. With recent cannabis legalization along with evidence indicating therapeutic benefits (e.g. chronic pain, chemotherapy-induced nausea, sleep disorders) [2], it seems practical to believe that marijuana use will continue to increase. Chronic marijuana use has led to patients presenting with complaints of nausea, vomiting and abdominal pain; an entity known as cannabinoid hyperemesis syndrome (CHS) [3].
As our society appears to be accepting recreational marijuana use, there have been a number of emergency room visits of individuals complaining of symptoms suggestive of CHS; these patients were ultimately found to have small bowel intussusception on computed tomography (CT) scan.
In this review, we hypothesize that there may be an association between cannabis use and transient adult intussusception (AI). We reviewed multiple cases of adult recreational marijuana users who presented with small bowel intussusception followed by a review of the literature.
The general approach to the management of AI trends toward an operative route, yet the majority of our patients were successfully managed conservatively. Our goal is to increase awareness and suspicion for when such patients present and review proposed mechanisms suggesting the association of cannabis in AI.
To our knowledge, there is very limited information in the scientific literature suggesting a relationship between cannabis use and intussusception.
MATERIALS AND METHODS
This is a case series of 11 patients who presented with an acute abdomen, subsequently diagnosed with small bowel intussusception on CT imaging. This series reviews patients from two community teaching hospitals over a 2-year period (2016–2018). There were no exclusion criteria. Patients were managed either conservatively or surgically. The aim of this series is to identify patients with increased risk for AI, discuss approaches in management and review mechanisms suggesting the association between cannabinoid (CB) use and intussusception in adults. A literature review was performed using PubMed, with search terms including intussusception, CB, marijuana and bowel obstruction. This report was exempted by institutional review board (IRB) committee of the affiliated facility.
RESULTS
There were 11 patients from two New York-based institutions diagnosed with intussusception and known to be marijuana users. There was almost equal gender distribution and the median age was 27 (range 18–38). One out of the 11 patients had diagnostic laparoscopy years prior for intussusception, and no lead point was found. The remaining 10 patients had no history of prior surgery, known intra-abdominal pathology or malignancy. The majority of patients (81%) presented with severe diffuse abdominal pain, and more than half (63%) presented with obstructive symptoms.
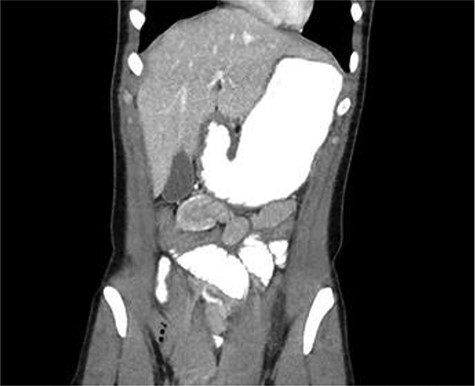
CT scan diagnosed 100% of the cases and all cases were reported as jejunojejunal (JJ) intussusception (Figs 1, 2). CT scan identified two patients having more than one intussuscepted segment. None of the patients were found to have lead points on imaging.
A 24-year-old female with CT scan with target sign in mid-right abdomen suggesting JJ intussusception

A 30-year-old male with CT scan with target sign in left upper quadrant suggesting JJ intussusception
Intervention was guided by each patient’s clinical picture at time of evaluation. Two patients underwent diagnostic laparoscopy, with one patient requiring laparoscopic reduction. The remaining patients were managed conservatively, with serial abdominal exams, resuscitation and pain management, and only two had nasogastric tube decompression.
The median length of stay was 2 days, with no significant difference in length of stay for those were where conservatively managed (mean = 2.4 days) compared to patients who underwent laparoscopic intervention (mean = 2.5 days). A summary of the clinical course and management of the patients in the case series is depicted in Table 1.
Case series included cases with patient’s demographics, clinical presentation, management and outcome
| Patient sex/age (year) . | Presenting symptoms . | Diagnostic modality . | Intussuscepted segment(s) . | Lead point . | Intervention . | Spontaneous resolution . | Length of stay (days) . |
|---|---|---|---|---|---|---|---|
| F/23 | Diffuse abdominal pain | CT scan | Jejunojejunal | None | Serial exams | Yes | 1 |
| F/30 | Abdominal pain | CT scan | Jejunojejunal (3 segments) | None | Serial exams | Yes | 3 |
| M/31 | RLQ pain | CT scan | Jejunojejunal | None | Serial exams | Yes | 1 |
| M/25 | Diffuse abdominal pain (+emesis) | CT scan | Jejunojejunal | None | Serial exams | Yes | 2 |
| M/38 | Abdominal pain | CT scan | Jejunojejunal (2 segments) | None | Serial exams | Yes | 6 |
| M/26 | Diffuse abdominal pain (+emesis) | CT scan | Jejunojejunal | None | Serial exams | Yes | 1 |
| M/30 | Diffuse abdominal pain (+emesis) | CT scan | Jejunojejunal | None | Diagnostic laparoscopy | Yes | 3 |
| F/18 | Diffuse abdominal pain (+emesis) | CT scan | Jejunojejunal | None | Diagnostic laparoscopy | Laparoscopically reduced | 2 |
| F/28 | LLQ pain (+emesis) | CT scan | Jejunojejunal | None | NGT | Yes | 3 |
| F/22 | Diffuse abdominal pain (+emesis) | CT scan | Jejunojejunal | None | NGT | Yes | 2 |
| M/26 | Diffuse abdominal pain(+emesis) | CT scan | Jejunojejunal | None | Serial exams | Yes | 1 |
| Patient sex/age (year) . | Presenting symptoms . | Diagnostic modality . | Intussuscepted segment(s) . | Lead point . | Intervention . | Spontaneous resolution . | Length of stay (days) . |
|---|---|---|---|---|---|---|---|
| F/23 | Diffuse abdominal pain | CT scan | Jejunojejunal | None | Serial exams | Yes | 1 |
| F/30 | Abdominal pain | CT scan | Jejunojejunal (3 segments) | None | Serial exams | Yes | 3 |
| M/31 | RLQ pain | CT scan | Jejunojejunal | None | Serial exams | Yes | 1 |
| M/25 | Diffuse abdominal pain (+emesis) | CT scan | Jejunojejunal | None | Serial exams | Yes | 2 |
| M/38 | Abdominal pain | CT scan | Jejunojejunal (2 segments) | None | Serial exams | Yes | 6 |
| M/26 | Diffuse abdominal pain (+emesis) | CT scan | Jejunojejunal | None | Serial exams | Yes | 1 |
| M/30 | Diffuse abdominal pain (+emesis) | CT scan | Jejunojejunal | None | Diagnostic laparoscopy | Yes | 3 |
| F/18 | Diffuse abdominal pain (+emesis) | CT scan | Jejunojejunal | None | Diagnostic laparoscopy | Laparoscopically reduced | 2 |
| F/28 | LLQ pain (+emesis) | CT scan | Jejunojejunal | None | NGT | Yes | 3 |
| F/22 | Diffuse abdominal pain (+emesis) | CT scan | Jejunojejunal | None | NGT | Yes | 2 |
| M/26 | Diffuse abdominal pain(+emesis) | CT scan | Jejunojejunal | None | Serial exams | Yes | 1 |
LLQ, left lower quadrant; NGT, nasogastric tube; RLQ, right lower quadrant.
Case series included cases with patient’s demographics, clinical presentation, management and outcome
| Patient sex/age (year) . | Presenting symptoms . | Diagnostic modality . | Intussuscepted segment(s) . | Lead point . | Intervention . | Spontaneous resolution . | Length of stay (days) . |
|---|---|---|---|---|---|---|---|
| F/23 | Diffuse abdominal pain | CT scan | Jejunojejunal | None | Serial exams | Yes | 1 |
| F/30 | Abdominal pain | CT scan | Jejunojejunal (3 segments) | None | Serial exams | Yes | 3 |
| M/31 | RLQ pain | CT scan | Jejunojejunal | None | Serial exams | Yes | 1 |
| M/25 | Diffuse abdominal pain (+emesis) | CT scan | Jejunojejunal | None | Serial exams | Yes | 2 |
| M/38 | Abdominal pain | CT scan | Jejunojejunal (2 segments) | None | Serial exams | Yes | 6 |
| M/26 | Diffuse abdominal pain (+emesis) | CT scan | Jejunojejunal | None | Serial exams | Yes | 1 |
| M/30 | Diffuse abdominal pain (+emesis) | CT scan | Jejunojejunal | None | Diagnostic laparoscopy | Yes | 3 |
| F/18 | Diffuse abdominal pain (+emesis) | CT scan | Jejunojejunal | None | Diagnostic laparoscopy | Laparoscopically reduced | 2 |
| F/28 | LLQ pain (+emesis) | CT scan | Jejunojejunal | None | NGT | Yes | 3 |
| F/22 | Diffuse abdominal pain (+emesis) | CT scan | Jejunojejunal | None | NGT | Yes | 2 |
| M/26 | Diffuse abdominal pain(+emesis) | CT scan | Jejunojejunal | None | Serial exams | Yes | 1 |
| Patient sex/age (year) . | Presenting symptoms . | Diagnostic modality . | Intussuscepted segment(s) . | Lead point . | Intervention . | Spontaneous resolution . | Length of stay (days) . |
|---|---|---|---|---|---|---|---|
| F/23 | Diffuse abdominal pain | CT scan | Jejunojejunal | None | Serial exams | Yes | 1 |
| F/30 | Abdominal pain | CT scan | Jejunojejunal (3 segments) | None | Serial exams | Yes | 3 |
| M/31 | RLQ pain | CT scan | Jejunojejunal | None | Serial exams | Yes | 1 |
| M/25 | Diffuse abdominal pain (+emesis) | CT scan | Jejunojejunal | None | Serial exams | Yes | 2 |
| M/38 | Abdominal pain | CT scan | Jejunojejunal (2 segments) | None | Serial exams | Yes | 6 |
| M/26 | Diffuse abdominal pain (+emesis) | CT scan | Jejunojejunal | None | Serial exams | Yes | 1 |
| M/30 | Diffuse abdominal pain (+emesis) | CT scan | Jejunojejunal | None | Diagnostic laparoscopy | Yes | 3 |
| F/18 | Diffuse abdominal pain (+emesis) | CT scan | Jejunojejunal | None | Diagnostic laparoscopy | Laparoscopically reduced | 2 |
| F/28 | LLQ pain (+emesis) | CT scan | Jejunojejunal | None | NGT | Yes | 3 |
| F/22 | Diffuse abdominal pain (+emesis) | CT scan | Jejunojejunal | None | NGT | Yes | 2 |
| M/26 | Diffuse abdominal pain(+emesis) | CT scan | Jejunojejunal | None | Serial exams | Yes | 1 |
LLQ, left lower quadrant; NGT, nasogastric tube; RLQ, right lower quadrant.
DISCUSSION
Intussusception is an uncommon process outside of the pediatric population and AI accounts for 5% of all small bowel obstructions. It occurs when one segment of bowel ‘telescopes’ into an adjacent segment, usually due to a lead point (secondary intussusception), resulting in potential obstruction and vascular compromise. The cause is usually benign in children and is managed by pneumatic or hydrostatic reduction with high success rates. In contrast, AI raises concern for tumors (≥65%) or other harboring pathology, whether intra-luminal or extra-luminal (e.g. diverticula, adhesions, polyps, celiac disease, Crohn’s disease) [4, 5]. An unknown cause (primary or idiopathic) in adults has been reported up to 20% of the time. CT is the best modality for diagnosis, showing sausage-shaped mass, target sign, vascular compromise and sometimes a lead point. Intussusception in adults has traditionally been highly associated with a malignant lead point and, thus, required surgical exploration. Due to such high tumor rates, the traditional approach to AI has been surgery; however, consideration to a more conservative management has been warranted more recently in the absence of warning signs [6, 7].
There are proposed mechanisms that explain the role of cannabis on intestinal function. These mechanisms attempt to describe the symptoms associated with CHS. CHS occurs in chronic marijuana smokers and is characterized by abdominal pain associated with intractable nausea and vomiting, often relieved by hot showers or smoking cessation [3]. Proposed mechanisms on a cellular level include G-coupled CB (CB1 and CB2) receptors located throughout the body producing various effects, i.e. the exogenous CB Δ9-tetrahydrocannabinol (THC) binds to CB1 receptors in the central nervous system leading to alterations in psychomotor behavior, appetite stimulation, as well as anti-emetic effects.
CB1 receptors located within the enteric nervous system, when stimulated by CBs, produce effects that include alterations in gastric and intestinal motility, decreased gastric emptying and LES relaxation [8, 9]. Exogenously applied CB receptor agonists inhibit enteric neuronal activity. In a publication by Boesmans et al. shows that CB1 receptor activation on myenteric neurons maintained in primary culture can suppress neuronal activity, presynaptic release of acetylcholine and mitochondrial transport along axons. They also provide initial evidence that myenteric neurons release endocannabinoids and which activate CB1 receptors constitutively [10]. As we develop a deeper understanding of these mechanisms and interactions, it seems reasonable to believe that both exogenous and endogenous CBs interacting with CB receptors may cause alterations in gut motility significant enough to cause an intussusception.
CONCLUSION
Our 11 cases have one common factor, which is chronic marijuana use. Our hypothesis that chronic marijuana use is associated with small bowel intussusception in adults is strengthened by the physiologic mechanisms produced by the interactions of THC and cannabidiol with CB receptors in the enteric nervous system. These are the same mechanisms proposed to explain CHS, which is traditionally a clinical diagnosis. Since these cases can present with spontaneous reduction, it is possible that small bowel AI is being under-diagnosed as CHS. The argument can be made that a link exists between CHS and small bowel AI or that they may be the same entity. Additionally, a review of scientific literature seems to show that obtaining a CT scan is of benefit in diagnosing AI and possibly ruling out a lead point. Furthermore, as many patients present with transient AI, the role of immediate surgical intervention in idiopathic adult small bowel intussusception is unclear. Our series indicates that non-operative and expectant management may be an acceptable approach with no significant change in length of stay. Future studies with randomized clinical trials for jejunojejunal intussusceptions in chronic marijuana smoker would provide stronger evidence in the management of these patients.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
No funding.
ETHICAL APPROVAL
Report was exempt from IRB approval by participating facility.



