-
PDF
- Split View
-
Views
-
Cite
Cite
Sabrina Barillas, Alejandra Rodas, Javier Ardebol, Juan Luis Martí, Nontraumatic chylothorax secondary to lymphoma and filariasis, Journal of Surgical Case Reports, Volume 2020, Issue 9, September 2020, rjaa309, https://doi.org/10.1093/jscr/rjaa309
Close - Share Icon Share
Abstract
Chylothorax is characterized by extravasation of chyle into the pleural space resulting from thoracic duct damage. The effusion is most commonly unilateral, with the right and left side being affected in 50% and 33.3% of the patients, respectively. Only 16.66% of cases present a bilateral effusion. The underlying etiology can be classified as spontaneous or traumatic. The diagnosis is made through pleural fluid analysis and imaging studies. The following article presents two cases of left spontaneous chylothorax: a 26-year-old male presenting with a chylous pleural effusion due to a non-Hodgkin lymphoma and a 47-year-old patient from a tropical area with a chylous pleural effusion attributed to filariasis. Filariasis as a cause of chylothorax is uncommon and there is not much literature on the topic. Alongside the case presentations, information on chylothorax etiology, mechanism, diagnosis and treatment options is provided.
INTRODUCTION
Chyle is a white, milky and yellowish substance that can be visualized macroscopically in less than half of the patients with chylothorax [1, 3]. Chylothorax is an effusion composed of chyle that accumulates within the pleural space secondary to thoracic duct damage or obstruction, which tends to be unilateral in most cases [1, 4]. Nearly 50–60% of chylous pleural effusions occur on the right side. Clinical presentation ranges from asymptomatic to symptoms similar to other forms of pleural effusions, including nonproductive cough and dyspnoea [2–4]. Fever and pleurisy are infrequent since chyle does not irritate pleural surfaces. The leading causes are trauma and malignancy. Diagnosis requires a pleural fluid analysis and radiological imaging, which includes chest radiography, computed tomography (CT) scans, lymphangiography and lymphoscintigraphy. The presence of chylomicrons in pleural fluid confirms the diagnosis [4]. The following cases consist of two patients who developed spontaneous chylothorax, one as a result of non-Hodgkin lymphoma and the other due to filariasis.
CASE PRESENTATION
The first case consists of a 26-year-old male that presented with dyspnoea at rest, tachycardia, jugular vein distention, and slight facial and upper limb edema. The patient had been previously treated with ceftriaxone and moxifloxacin, and underwent a left thoracostomy due to a chest radiograph that showed a pleural effusion in the left inferior hemithorax. At auscultation, the patient had reduced air entry in the left lung base. The patient did not show improvement with the treatment previously given, so new laboratory tests were ordered. The blood test showed an elevated lactate dehydrogenase at 652 U/L and the pleural fluid analysis showed an elevated lactate dehydrogenase at 911 U/L, cholesterol level at 46 mg/dl, and triglyceride level at 847 mg/dl. According to these results, the pleural effusion was classified as an exudate. The high triglyceride level was consistent with a chylous effusion. A chest CT confirmed a pericardial effusion, the previously noticed free pleural effusion, and an irregular mass in the anterior mediastinum with heterogeneous density that included hypodense areas that suggest necrosis (Figs 1 and 2). Subsequently, the patient underwent surgical treatment, which consisted of a pericardial window. Aside from this procedure, the anterior mass was biopsied. Histological analysis revealed a non-Hodgkin lymphoma. Due to the diagnosis, the patient was transferred to the hematology care unit to receive chemotherapy, but he continued to deteriorate and passed away 2 months later.
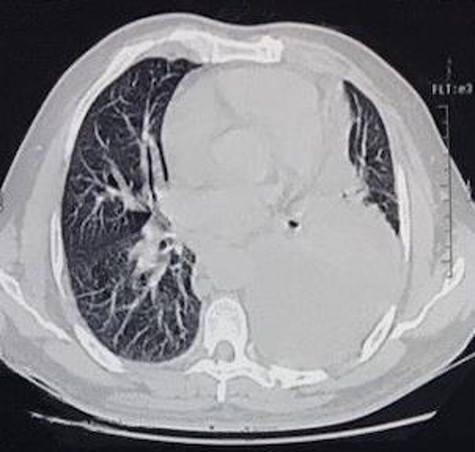
CT scan axial view of anterior mediastinal mass, left lung free pleural effusion and intercostal drainage.
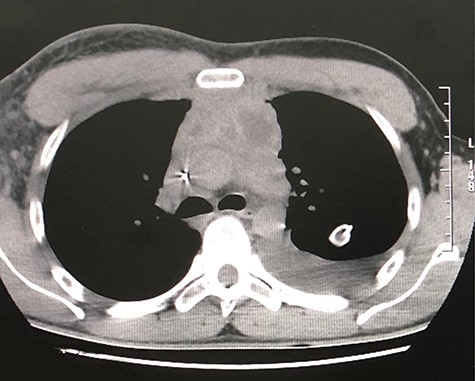
CT scan axial view of a pericardial and left lung pleural effusion.
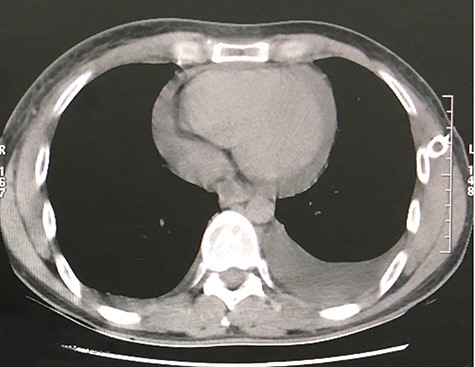
The second case consists of a 47-year-old male from a rural location in Guatemala that presented with malaise, fever, nausea, vomiting and left chest pain, described as oppressive that irradiates toward the neck. The pain got worse while being on supine position. The patient was previously treated with antibiotics and underwent a left thoracostomy due to a chest radiograph that showed a pleural effusion in the lung base (Fig. 3). On chest auscultation and percussion, air entry was reduced and dullness was perceived in the left lung base, respectively. Due to these findings, laboratory tests were ordered. The blood test showed an elevated lactate dehydrogenase at 156 U/L and the pleural fluid analysis showed an elevated lactate dehydrogenase at 1282 U/L, cholesterol level at 66 mg/dl, triglyceride level at 128 mg/dl, presence of Klebsiella pneumoniae and a hematoxylin stain positive for helminth larvae. According to these results, the pleural effusion was classified as an exudate. The high triglyceride level was consistent with a chylous effusion. A chest CT showed left loculated pleural effusion, cardiomegaly, slight pericardial effusion and mediastinal adenomegaly (Fig. 4). The patient presented full recovery after surgical and medical treatment.
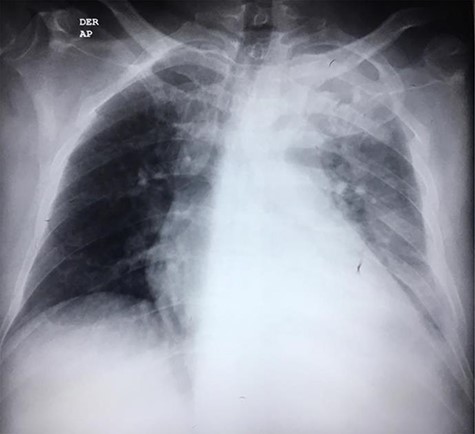
CT scan axial view of left pleural effusion, cardiomegaly and pericardial effusion.
DISCUSSION
Chylothorax is characterized by accumulation of chyle in the pleural cavities that results from thoracic duct damage [2, 4]. The etiology can be classified as spontaneous (nontraumatic) and traumatic. Traumatic chylothorax accounts for more than 50% of all cases, being thoracic surgery the leading cause [5]. Malignant lymphoma is the most common cause of nontraumatic chylothorax, with non-Hodgkin lymphoma having a higher prevalence. Other nontraumatic chylothorax etiologies include sarcoidosis, amyloidosis, superior vena cava thrombosis, congenital duct abnormalities and diseases that affect lymph vessels. Mortality for traumatic chylous pleural effusion is 50% and nontraumatic cases are often fatal [1, 3, 5]. Chylothorax can be treated with a conservative approach, radiologic interventions and surgery. Conservative treatment consists of diet and nutrient replacement, use of somatostatin and octreotide to reduce chyle production, thoracocentesis and drainage to improve pulmonary function and treatment of the underlying disease. Radiologic interventions include transjugular intrahepatic stent shunt, lymphography, percutaneous closure of the thoracic duct and percutaneous needle disruption of lymphatic pathways. Surgery is recommended if there has been a rapid deterioration of the patient’s nutritional status with conservative treatment alone. Surgical interventions include thoracic duct ligation and pleurodesis [3, 4, 6].
In the first case, due to the patient’s lack of significant background and trauma history a chest CT was ordered. The patient’s age and the anterior mediastinal mass confirmed by the chest CT raised suspicion of a lymphoma, so a biopsy was performed. Histological analysis revealed a non-Hodgkin lymphoma. According to this result, chylothorax most likely developed due to compression of the thoracic duct by the lymphoma. The patient’s adequate treatment consisted of chemotherapy, hence he was referred to the hematology care unit.
In the second case, the patient’s symptomatology, absence of trauma history and his place of residence suggested an infectious etiology. Evidence of a pleural effusion in a chest radiography led to performing a thoracentesis that revealed the presence of a chylothorax, helminth larvae and eosinophils. A chest CT confirmed the absence of malignancy. According to these results, chylothorax most likely developed due to obstruction of the thoracic duct by microfilaria. This diagnosis is also supported by the fact that Guatemala is a tropical country where helminths as Wuchereria bancrofti predominate [7]. The underlying disease was treated with diethylcarbamazine, and the surgical intervention consisted of a pleural toilette through video-assisted thoracoscopic surgery and chylothorax drainage. After these procedures, the patient recovered.
CONCLUSION
Chylothorax is an unusual manifestation of filariasis, yet clinicians must have a high index of suspicion whenever a patient comes from an endemic area [8]. These cases are of interest as the background upon which both patients developed chylothoraces is rare. Diagnosis should take into account the patient’s clinical presentation, as well as laboratory and imaging findings. Dyspnoea, reduced air entry and dullness in the lung are not pathognomonic of chylous pleural effusion, but should raise suspicion when associated with malignancy or trauma history. There is not enough evidence of the optimal management but a conservative approach is suggested. Restricting a fatty diet is also important. Surgical intervention should be withheld unless indicated. The patients’ treatment was managed by a multidisciplinary team and mainly consisted of treating the underlying disease and relieving symptoms. Early diagnosis and treatment is recommended in order to avoid complications such as nutritional and immunological depletion.
CONFLICT OF INTEREST STATEMENT
None declared.



