-
PDF
- Split View
-
Views
-
Cite
Cite
Shingo Kunioka, Kishu Fujita, Shizuko Iwasa, Hironori Murakami, Hiroyuki Kamiya, Kenji Yamazaki, Hiroyuki Tsukui, A rare form of cardiac myxoma: interatrial septum tumor, Journal of Surgical Case Reports, Volume 2020, Issue 9, September 2020, rjaa333, https://doi.org/10.1093/jscr/rjaa333
Close - Share Icon Share
Abstract
A myxoma is one of the most common tumors in cardiac surgery, with most of them originating from the left or right atrial walls and causing embolic complications. An 84-year-old woman was referred to our institution after echocardiography showed an interatrial septum tumor that was presumed to be a thrombus; however, postoperative pathological examination revealed it to be a cardiac myxoma. This atypical myxoma was covered with a solid capsule containing connective tissue and substantial calcifications, which had made it difficult to establish a diagnosis of myxoma.
INTRODUCTION
A myxoma is the most common cardiac tumor located in the left atrium in ~75–90% of cases [1, 2]. Most patients present with one or more of the triad of embolism, intracardiac obstruction and constitutional symptoms. Centofanti et al. [2] reported that 71% of patients with myxomas had congestive heart failure or palpitation or both, 23% had embolic disease and 20% had neurological symptoms. Echocardiography is the most reliable diagnostic modality for cardiac myxomas and shows typical findings including fibroelastic morphology, mobility and stalk in some cases. In this case, however, the tumor located in the interatrial septum (IAS) was diagnosed as a thrombus rather than a myxoma preoperatively because there was no mobility or stalk and owing to the atypical location of the mass [3]. However, postoperative histological examination confirmed it as a cardiac myxoma.
CASE REPORT
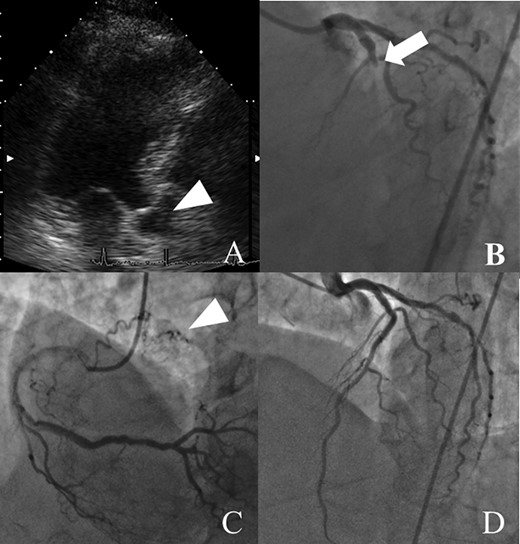
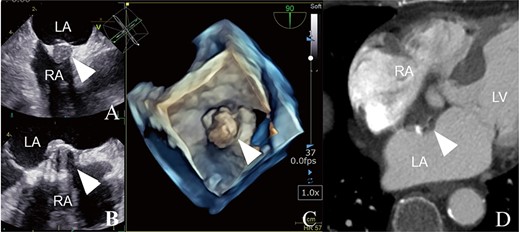
An 84-year-old woman was referred to our institution because of an IAS tumor detected on follow-up echocardiography (Fig. 1A). She had a history of acute myocardial infarction (MI) at the age of 73 years. Although she had few coronary risks, the left anterior descending (LAD) artery was totally occluded at the proximal segment (Fig. 1B). Further, no arteriosclerosis was found in other coronary arteries (Fig. 1C). Percutaneous coronary intervention was successfully performed, and follow-up coronary arteriography (CAG) showed no restenosis (Fig. 1D). She had no symptoms of congestive heart failure or murmur; however, transthoracic echocardiography incidentally revealed an IAS tumor presenting as a solid and immovable mass of 14 × 16 × 12.1 mm, while transesophageal echocardiography showed an IAS solid tumor with calcification (Fig. 2A–C). Enhanced computed tomography revealed a low-density area with a spot of high density, leading to suspicion of a cardiac cyst, thrombus or myxoma (Fig. 2D). Our cardiac team concluded that tumor pathological examination was necessary for an accurate diagnosis.
Preoperative examination findings (A–C): trans-esophageal echocardiography findings. (D) Enhanced computed tomography findings. Each image shows an IAS tumor with a solid mass and calcification suggesting a thrombotic IAS tumor (arrowheads). LA, left atrium; RA, right atrium; LV, left ventricle.
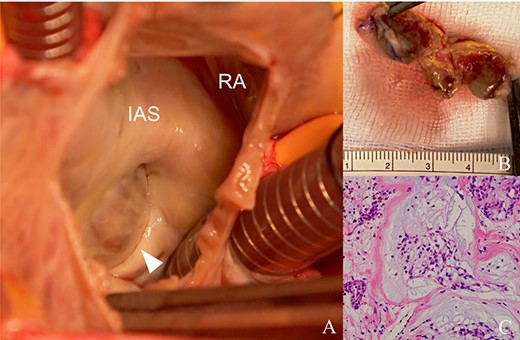
Intra- and postoperative histological findings. (A) Trans-right atrial view. The tumor is attached to the IAS wall. (B) The hard capsule with calcification. (C) Pathological findings. Concentric arrangement of cells around vascular cells, which is typical of myxomas.
Surgical tumor resection was performed under standard cardiac arrest via median sternotomy. The tumor was located at the fossa ovalis and was black-brown (Fig. 3A). The boundary between the tumor and healthy cardiac tissue was clear because the tumor was surrounded by solid connective tissue, with severe calcification (Fig. 3B). After tumor resection, an atrial septal defect was closed with a polytetrafluoroethylene patch (φ25 mm). The postoperative course was uneventful. Postoperative transthoracic echocardiography showed no residual tumors or shunt. Pathological examination revealed that the tumor was a myxoma (Fig. 3C).
Preoperative findings before percutaneous coronary artery intervention. (A) CAG shows the totally occluded left coronary artery suggesting embolization by thrombus or tumor (arrow). (B) Follow-up CAG shows no signs of arteriosclerosis, such as diffuse constriction. (C, D) Six years before presentation, right coronary artery angiography shows a tumor with feeding vessels, and echocardiography shows an IAS tumor (arrowheads), suggesting that the tumor was present at that time.
COMMENT
We encountered a case of typical IAS myxoma that was difficult to differentiate from a thrombus or malignant tumor using only preoperative echocardiography and computed tomography. Approximately 75–90% of cardiac tumors are benign, whereas the remaining are malignant [1, 2]. Further, ~75% of myxomas occur in the left atrium and 25% in the right atrium [4]. Most IAS tumors are found during percutaneous closure of a patent foramen ovale [5].
Transesophageal echocardiography has high diagnostic specificity and sensitivity for cardiac tumor [2]; the differentiation is difficult due to their similar presentations on imaging. Furthermore, a thrombus may have a stalk [6]. We suspected the tumor to be a thrombus rather than a myxoma or another malignant tumor because it was solid and surrounded by calcification. Postoperative histological examination, however, concluded that it was a myxoma, indicated by the presence of an extracellular matrix of abundant myxoma cells clustered in rudimentary vascular formations (Fig. 3C).
Myxomas can cause cardiac obstruction and distal embolization; however, the indication for surgery remains controversial [1]. Our cardiac team had discussions with the patient and her family to ascertain the tumor’s origin, which was not clear due to its unusual location. Half of the primary tumors of the right atrium are malignant, whereas most of those of the left atrium are benign, and a majority is myxomas (50–75%) [7]. Dimitrova et al. reported a large myxoma comprising lymphoid cells. However, the prevalence of malignant IAS tumors remains unclear.
Retrospectively, the patient’s past medical history suggested a myxoma. The patient was healthy with few coronary risk factors; however, she had experienced an acute MI 6 years before surgery. CAG had shown an intact coronary artery, except for total occlusion of the proximal LAD (Fig. 1A). Follow-up CAG showed no restenosis of the LAD and intact distal LAD (Fig. 1D). These findings suggest that the patient had an acute MI due to myxoma embolization rather than atherosclerotic disease and showed a pale contrast effect suggesting the presence of feeding vessels of a tumor (Fig. 1C). We thus speculate that the myxoma had existed from before and caused acute MI.
CONSENT TO PUBLISH
The participant has consented to the submission of the case report to the journal.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



