-
PDF
- Split View
-
Views
-
Cite
Cite
Muhammad Abu-Rmaileh, Hanna Jensen, Mary Katherine Kimbrough, Traumatic bilateral ureteral tear in a pregnant woman after a motor vehicle crash: a case report, Journal of Surgical Case Reports, Volume 2020, Issue 9, September 2020, rjaa331, https://doi.org/10.1093/jscr/rjaa331
Close - Share Icon Share
Abstract
Bilateral ureteropelvic junction (UPJ) tears are rare. Trauma can obscure this diagnosis. The objective of this case report is to highlight the rapid diagnosis of this injury and care in the case of pregnancy. A 22-year-old pregnant female was ejected from her car and presented with abdominal pain. The patient got a computed tomography (CT)-chest, abdomen, pelvis (CT-CAP) revealing bilateral ureteral injury, which was confirmed on retrograde cystoscopy. Her injuries were treated with nephrostomy tubes with plans for definitive repair after pregnancy. Fetus remained stable throughout her care and the patient was discharged with no complications. Due to the rapid diagnosis and effective stabilization, the patient and fetus recovered well from the injuries and multiple procedures. While there are many explanations for bilateral UPJ tears, deceleration and hyperextension seem to be the two major mechanisms of this injury.
INTRODUCTION
Ureteral injuries are commonly missed in trauma. Possible reasons for this include prioritization of severe injuries, hemodynamic instability preventing radiographic imaging or low clinical concern due to misperception that the retroperitoneal location of ureters is completely protective [1,2]. Usually, injuries are associated with traumatic pelvic fractures or penetrating injuries and are limited to one ureter; however, we present a case where the patient experienced complete, bilateral ureteral injury without any associated pelvic fracture.
CASE PRESENTATION
A 22-year old female with a 12-week intrauterine pregnancy (IUP) presented to our emergency department (ED) after a motor vehicle crash (MVC) rollover with ejection. She was not wearing a seat belt. The patient was hit by another car at ~50 mph on the highway, ejected out of the vehicle, and lost consciousness.
On the scene, the paramedics reported a Glasgow Coma Scale (GCS) of 14 with a heart rate of 103 bpm and a systolic blood pressure of 86 mmHg. She was placed in a cervical collar and airlifted to our facility. In the ED, her initial vitals were recorded as 94/64 mmHg, pulse of 105 bpm, respiratory rate of 20 and breathing room air with 100% oxygen saturation. Her airway was patent, and she presented with bilateral breath sounds. Radial and pedal pulses were symmetric. The patient reported neck, back and pelvic pain. Physical exam showed various lacerations and abrasions on her abdomen consistent with motor vehicle ejection in addition to periorbital swelling, right shoulder bruising and Grey-Turner sign. She did not have peritonitis on the exam.


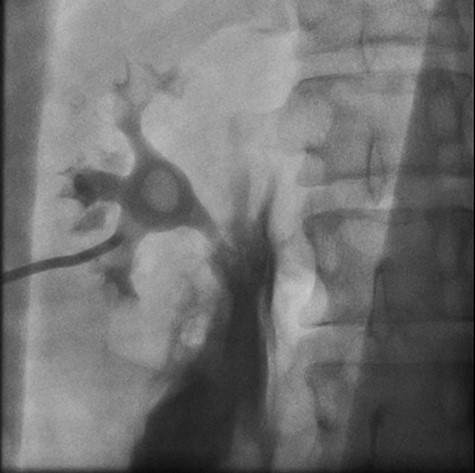
Right retrograde cystoscopy exhibiting extravasation of contrast.

Left retrograde cystoscopy exhibiting extravasation of contrast.
Fetal HR was measured at 135 bpm. Chest X-ray revealed a small apical pneumothorax and a fractured right clavicle. She was taken to the computed tomography (CT) scanner where CT-CAP with contrast revealed a Grade 2 liver laceration, Grade 3 splenic laceration and bilateral Grade 4 kidney injuries with extravasation of contrast on the renal delay, suggestive of urine extravasation. No pelvic fracture was found on imaging (Figs 1 and 2).
Cystoscopy with retrograde pyelogram was performed by the urology team and this showed total disruption of the UPJ bilaterally with extravasation of contrast (Figs 3 and 4). She underwent bilateral interventional radiology nephrostomy tube placement. The definitive repair was planned for after pregnancy, but she required tube changes every 6 weeks. There was no fetal distress during her stay. She recovered well and was discharged after 5 days.
DISCUSSION
Ureteral injuries secondary to trauma are frequently missed. Often ureteral injury is low on physicians’ differential diagnosis and can be missed up to 36 h after the trauma [3]. Blunt traumatic ureteral injuries are often associated with pelvic and lumbosacral fractures; however, this case shows that even without pelvic or lumbosacral trauma, patients can still present with major ureteral trauma with a blunt mechanism [3, 4].
In general, ureteral injuries may occur more frequently in children due to the small amount of perinephric fat surrounding the kidney and ureter [3]. The smaller amount of fat decreases protection to the kidney and ureter and allows increased mobility of the kidney relative to the ureter. An acceleration-deceleration mechanism can cause tearing or shearing of the ureters due to changes in momentum [1]. Another suggested mechanism for injury is extreme hyperextension of the ureter against the vertebral column, which can explain bilateral ureteral tears regardless of the presence of lumbar fracture [4, 5]. Other possible causes of this injury can be directly related to the mechanism of injury, such as direct compression of the kidney and ureter from the weight of a vehicle, direct impact from a back-blow in an assault, or from an adjacent bony fragment causing ureter laceration. In this case, the gravid uterus could have placed some tension on the ureters, leading to the UPJ injuries during an acceleration-deceleration or hyperextension mechanism.
Pregnant women have three times the mortality of non-pregnant women in trauma. Physiologic changes can complicate the primary survey assessment in trauma; most of these changes did not impact our patient’s care since she was only 12 weeks. Fetal mortality can be as high as 61% in major traumas [6, 7]. Best predictors for fetal outcomes include changes in fetal heart rate monitored by fetal heart tones (M-Mode on bedside ultrasound if under 23 weeks) and external fetal monitoring if 23 weeks or over [8, 9]. A possible explanation for the preservation of pregnancy, in this case, could be that the early gravid uterus was still located in the pelvis at 12 weeks, which protected the uterus and fetus from the energy transmitted to the patient’s abdomen in the crash. Additionally, her injuries were able to be managed either non-operatively or with minimally invasive approaches rather than an invasive laparotomy. While the fetus was exposed to radiation and physiologic stress, the patient was able to avoid a laparotomy which can be associated with adverse pregnancy outcomes and fetal demise [10].
ACKNOWLEDGEMENT
We would like to thank the Department of Trauma and General Surgery at the University of Arkansas for Medical Sciences for all their help.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None declared.



