-
PDF
- Split View
-
Views
-
Cite
Cite
Nawaf Abdulkareem Alomary, Majid Zaab Albeeshi, Rasha Eidah Al Thebaity, Zeyad Mohammed Yousef, Sami Abdelkereim El-Boghdadly, Aggressive angiomyxoma persistently misdiagnosed as an obturator hernia managed with resection and hormonal therapy: case report, Journal of Surgical Case Reports, Volume 2020, Issue 9, September 2020, rjaa330, https://doi.org/10.1093/jscr/rjaa330
Close - Share Icon Share
Abstract
Aggressive angiomyxoma (AA) is an uncommon mesenchymal tumor that mainly affects the perineum and pelvis in females of reproductive age. AA is commonly misdiagnosed as a Bartholin’s duct cyst, abscess or levator hernia. A 42-year-old female presented with a large, progressive and painless perineal swelling. She was initially diagnosed with an obturator hernia three times over the past 10 years and underwent multiple surgeries for recurrences. For this presentation, she underwent exploratory laparotomy. No hernia was identified. A large mass over the perineal area extending from the vulvar commissure to the anus was visualized. The diagnosis of AA was made on histopathology. Leuprolide (GnRHa) was used as hormonal therapy postoperatively. AA should be considered in any pelvic mass in a young female that recurs after excision. Prompt diagnosis will contribute toward minimizing local destruction of surrounding structures.
INTRODUCTION
Aggressive angiomyxoma (AA) was first described by Steeper and Rosai in 1983 as a soft-tissue mass that mostly occurs in the pelvis and perineum, with a female-to-male ratio of ~6:1. [1,2] Prevalence is undetermined due to the rarity of the condition, which makes management and counseling difficult [3]. AAs are characterized by their large size, and their noncapsulated, locally infiltrative nature. [4] Although it is a slow-growing tumor with a low metastatic capacity, it has a great tendency for local recurrence [2]. Wide local excision with tumor-free margins is the mainstay of surgical management [4]. We report the case of a 42-year-old female with a large, AA over the perineal area that was misdiagnosed and operated three times over the past 10 years before being correctly diagnosed and managed.
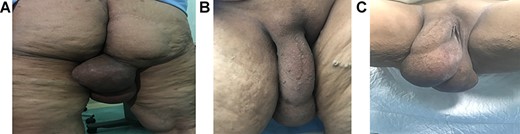
Gross images of the mass in a standing view showing the relations to the vulva and gluteal regions, (A) posterior view showing the scar from a previous surgery in the right gluteal area and the extension of the mass, (B) anterior view in a standing position and (C) lithotomy, respectively.
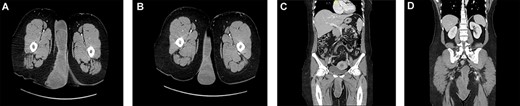
Multiple cuts of a CT abdomen and pelvis scan showing a multicompartmental, multilobulated, low pelvic and perineal soft-tissue lesion, with heterogeneous enhancement, measuring almost 21 × 17 × 5 cm.
CASE PRESENTATION
A 42-year-old anemic female presented to the clinic, complaining of a recurrent obturator hernia for the past 10 years. It was a large, painless, progressive swelling in the perineum, involving the labial fold. There were no bowel obstruction symptoms. She was previously operated for the hernia three times in different centers. On examination, there was a large swelling extending from the right medial gluteal area to the right labial fold measuring 20 × 15 cm. It was nontender and had a firm consistency, with no overlying skin changes (Fig. 1). Laboratory investigations were within normal limits. Computed tomography (CT) scans of the abdomen and pelvis showed a massive, multicompartmental, multilobulated soft-tissue lesion in the lower pelvis and perineum, exerting a mild mass effect (Fig. 2). Perineal mass excision, possible mesh placement and stoma creation was planned. At exploratory laparotomy, the abdominal and pelvic cavities were examined. There was no evidence of a defect or hernia. The extraperitoneal space was explored and the obturator foramen was identified without any hernia. The procedure then shifted to excision of the mass. It was lobulated within a capsule and extending from the vulvar commissure to the anus. It was also involving part of the lateral vaginal wall, the lower part of the rectum and anal canal which needed to be excised (Fig. 3). The mass was directly subdermal at the vulvar commissure site, so part of the labia minora skin was excised with the mass. The vaginal wall was repaired by a urogynecologist. The rectum was repaired by the primary surgeon. A diversion end sigmoid colostomy was created. Wound closure was assisted by plastic surgery. No tissue or skin coverage was required. The histopathological report revealed an AA extending to the margins with ulcerated and reactive skin tissue. Immunostaining for estrogen and progesterone were both positive. The postoperative course was uneventful. At 8 months follow-up, abdomen and pelvis CT concluded that there was a minimal residual perineal mass without extension to the pelvis. Following discussion in the multidisciplinary tumor board, she was started on hormonal therapy after ~1 year of surgery with leuprolide 22.5 mg, intramuscular, every 3 months. Hormonal therapy was continued for a total of 15 months with frequent follow-up images which showed no change in the residual mass. She underwent colostomy reversal 3 years after and was doing well on regular follow-ups. The patient consented to the publication of this case report with images. All measures were taken to ensure her privacy and anonymity.
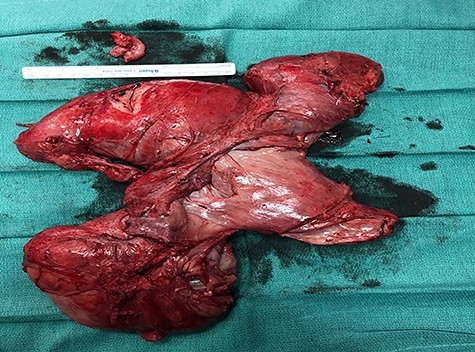
Excised specimen, soft-tissue mass consisting of an irregular piece of red-tan soft to firm tissue, measuring 31.5 × 20.0 × 0.8 cm along with overlying skin (not shown).
DISCUSSION
AA is an uncommon mesenchymal tumor that mainly arises from the perineum and pelvis in females of reproductive age [5]. Patients who suffer from AA can have a variable presentation, from a large pelvic mass diagnosed on imaging, to an asymptomatic vulvar or perineal nodule [4]. The most encountered presentation of AA is a vaginal or vulvar soft mass, usually misdiagnosed as a Bartholin’s duct cyst, vulvar mass, lipoma, vulvar abscess, vaginal cyst, Gardner’s duct cyst, vaginal prolapse or levator hernia [6]. Misdiagnosed cases of AA have been reported to be as high as 82% [3]. Definitive diagnosis is made on the basis of histopathological features, typically stellate and spindle cells with poorly demarcated cytoplasm, separated by loose myxoid stroma abundant in collagen fibrils [4]. AA is a benign tumor, but due to the high rate of local recurrence after surgery, it is characterized as aggressive [7]. The tumor is hormone-sensitive, as it expresses estrogen and progesterone receptors [2]. Primary surgery for AA is frequently extensive, due to the local invasion of the tumor into the surrounding tissue. Furthermore, the recurrence rate is not associated with the surgical margin status [8]. Recurrence of the tumor usually happens within the first 5 years after the initial surgery, however recurrences were reported as far as 14 years after initial resection in some studies [9]. In this case, the patient presented with a fourth recurrence, and similar to other cases, it was misdiagnosed. The initial diagnosis was obturator hernia, which resembles AA in that both of them are hard to diagnose, predominant in females, and present with a palpable mass in the groin [5,10]. However, this patient did not have any signs of intestinal obstruction or pain in the middle aspect of the thigh (Howship–Romberg sign). Although there was intraoperative suspicion, final diagnosis was only confirmed postoperatively. Due to the variability in location and size of AA, there is no standardized surgical procedure, and each surgical treatment should be individualized to the case [4]. In this case, part of the skin from the labia minora, and part of the rectal and vaginal walls were excised. If suspicious for recurrence, examination accompanied by imaging should be included in follow-up surveillance [4]. As in this case and other reported cases, hormonal therapy is an alternative method of treatment with a different variation of response [2]. In this case, hormonal therapy with leuprolide was used postoperatively as the preoperative diagnosis was uncertain. In the literature, gonadotrophic-releasing hormone agonists (GnRHa) are said to be the first-line hormonal therapy, and in some cases, it can be definitive treatment [2].
CONCLUSION
AA is a rare condition with a high rate of recurrence. Due to the rarity of this condition, misdiagnosis is very common. Knowledge of its characteristics and an index of suspicion will allow clinicians to provide these patients with the necessary treatment, through earlier diagnosis.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
References
- myxoma
- edema
- abscess
- cysts
- hernias
- hernia, obturator
- leuprolide
- anogenital region
- reproductive physiological process
- surgical procedures, operative
- anus
- diagnosis
- neoplasms
- pelvis
- vulva
- pelvic mass
- bartholin's gland duct
- endocrine therapy
- gonadotropin-releasing hormone analogs
- laparotomy, exploratory
- misdiagnosis
- excision
- histopathology tests



