-
PDF
- Split View
-
Views
-
Cite
Cite
Mohammed Ibrahim, Bernd Linsmeier, Lung herniation through the thoracic wall after persistent sneezing and coughing in an obesity and COPD Patient, Journal of Surgical Case Reports, Volume 2020, Issue 9, September 2020, rjaa303, https://doi.org/10.1093/jscr/rjaa303
Close - Share Icon Share
Abstract
We present the case of a 61-year-old male patient with a known medical history of morbid obesity, chronic obstructive pulmonary disease and atrial fibrillation, who was receiving anticoagulation therapy with enoxaparin natrium prescribed by his family physician. The patient presented himself to the emergency department of our hospital with a complaint of severe pain in the right hemithorax, dyspnea, and diffuse cutaneous and subcutaneous haematoma in the inferior part of the right hemithoracic region. The patient underwent right-side video-assisted thoracic surgery on the second day to evacuate the haematothorax. Thoracic wall repair was achieved using a sandwich technique with a sublay reinforced with pericostal sutures and onlay insertion of bovine pericardium mesh.
INTRODUCTION
Spontaneous lung hernia is a rare disease that presents as a protrusion of the lung parenchyma through the thoracic wall without trauma or pathologic process. It typically occurs after persistent sneezing and coughing and involves intercostal muscle weakness or defect. The condition may be associated with morbid obesity, chronic obstructive pulmonary disease (COPD), diabetes mellitus and steroid use [1–3].
Lung herniation was first classified by Morel-Lavallee in 1847 [2, 4–6]. The classification of lung herniations is based on the anatomical position of the defect (Table 1).
The first case of extrathoracic herniation of the lung was reported by Roland in 1499 [5]. Brock and Heitmiller [3] have reported 16 cases of spontaneous lung herniation due to coughing, sneezing or sudden abnormal movement in the absence of trauma. Most of the patients were suffering from morbid obesity.
Traumatic hernias most commonly occur after thoracic surgical approaches such as thoracotomies and video-assisted thoracoscopies (VATS), while acquired spontaneous defects are caused by coughing and sneezing (or any activity that increases intrathoracic pressure), typically in patients with COPD and/or prolonged therapy with steroids [1–3].
CASE REPORT INTRODUCTION
A 61-year-old male patient with a known medical history of morbid obesity, COPD and atrial fibrillation, who was receiving anticoagulation therapy with enoxaparin natrium presented himself to the emergency department of our hospital with a complaint of severe pain in the right hemithorax, dyspnoea and diffuse cutaneous and subcutaneous haematoma in the inferior part of the right hemithorax.
| Anatomic . | Etiologic . |
|---|---|
| Diaphram | Spontaneous |
| Intercostal cervical | Secondary |
| - Congenital | |
| - Acquired: traumatic spontaneous | |
| - Pathologic: inflammation or neoplasm |
| Anatomic . | Etiologic . |
|---|---|
| Diaphram | Spontaneous |
| Intercostal cervical | Secondary |
| - Congenital | |
| - Acquired: traumatic spontaneous | |
| - Pathologic: inflammation or neoplasm |
| Anatomic . | Etiologic . |
|---|---|
| Diaphram | Spontaneous |
| Intercostal cervical | Secondary |
| - Congenital | |
| - Acquired: traumatic spontaneous | |
| - Pathologic: inflammation or neoplasm |
| Anatomic . | Etiologic . |
|---|---|
| Diaphram | Spontaneous |
| Intercostal cervical | Secondary |
| - Congenital | |
| - Acquired: traumatic spontaneous | |
| - Pathologic: inflammation or neoplasm |
The patient reported persistent sneezing and coughing. Some hours later, he developed increased dyspnoea (initially on exertion and then, during rest), a local haematoma, a subcutaneous movable balloon-like mass exacerbated by breathing and severe pain in the inferior ventrolateral area of the right hemithorax.
Physical examination revealed a localized movable soft tissue mass on the right side of the thorax. Chest radiography showed hazy airspace opacity, highly suspicious for lung herniation (Fig. 1).
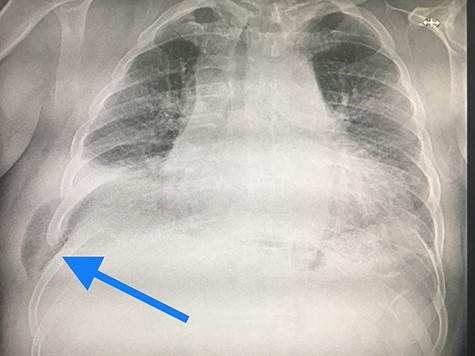
Chest radiography showed hazy airspace opacity, highly suspicious for lung herniation.
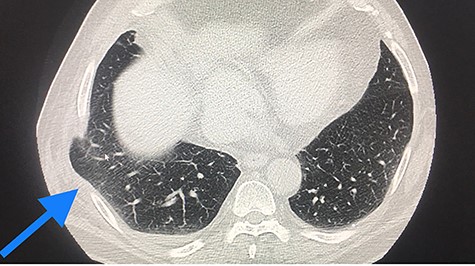
CT scan, lung herniation in the right hemithoracic, with clear position of the lung between the ribs and under the muscle straits.
Thoracic computed tomography (CT) scan showed a pulmonary hernia in the seventh intercostal space (ICS) due to a defect in the chest wall, minimal haematothorax, lung emphysema, but no pulmonary nodules and no skin or mediastinal emphysema (Fig. 2).
We performed surgical therapy as follows:
Video-assisted thoracoscopy to evacuate the haematothorax and accurately localize the hernia position.
A small skin incision was made on the exact location of the lung hernia cutaneous, subcutaneous and muscles states preparation followed. Using a sandwich technique, we inserted a sublay bovine pericardium mesh reinforced with pericostal sutures, followed by onlay mesh placement. Redon 16 catheters were placed, and the incision was closed with continuous sutures (Fig. 3a–c).

(a) Insertion of the bovine pericardium mesh in sublay position and fixtation with continuous sutures, (b) the reinforced chest wall closure with pericostal sutures and (c) the onlay Insertion of the bovine pericardium mesh and the insertion of Redon catheters over the sublay inserted mesh and under the ICS.
Finally, the chest tube was connected to the Suction System −20 cm H2O, and both Redon catheters were connected to suction pressure plastic bottles.
DISCUSSION
Lung hernia repair procedures are frequently used in thoracic surgery. Different approaches have been reported, and most of them are applied through an open thoracotomy using a single insertion for the mesh on onlay position.
Reardon et al. [7] described a minimally invasive technique to repair lung hernias. Our team successfully modified the surgical procedure as follows:
We used a VATS approach to localize the hernia and evaluate the size and type of the defect, followed by an accurate external incision over the hernia. We applied a sandwich technique to insert a sublay and onlay mesh. The chest wall was reinforced with several pericostal sutures [6].
Chest wall reconstruction can also be achieved with rotational muscle flaps and omentum combined with mesh insertion in case of inadequate muscle and subcutaneous layers [3, 6, 8].
Biological meshes such as bovine pericardium mesh [3, 6, 8] and synthetic meshes such as polytetrafluoroethylene (Vicryl Ethicon, Sommerville, NJ), polypropylene [3, 7, 8] or Gore-Tex® Dual Mesh [9] are widely used.
CONCLUSION
Surgical management of lung herniation can avoid further complications such as pain, ischaemia of the lung parenchyma secondary to torsion, lung contusion, dyspnoea and future chest wall instability.
From our single-case experience, we decided to perform a sandwich method using sublay and onlay mesh insertion with biomaterials such as fascia lata or bovine pericardium patches, which can be accepted by the human body, avoiding wound seroma. Wound closure was achieved with pericostal sutures, followed by continuous sutures for the muscle, subcutaneous and cutaneous layers.
Surgical approaches may vary, but the primary objective is to achieve closure of chest wall defects by applying a mesh in sublay or onlay position or combined with a sandwich method. The use of direct pericostal sutures only is also considered acceptable [3, 6].
CONFLICT OF INTEREST STATEMENT
The authors declare that there is no conflict of interest.
ETHICAL APPROVAL
Not applicable.
References
- anticoagulation
- atrial fibrillation
- obesity
- pericardial sac
- enoxaparin
- chronic obstructive airway disease
- dyspnea
- cough
- hematoma
- cattle
- emergency service, hospital
- obesity, morbid
- pain
- physicians, family
- sneezing
- surgical mesh
- sutures
- thoracic surgery, video-assisted
- medical history
- persistence
- chest wall
- lung hernias
- chief complaint



