-
PDF
- Split View
-
Views
-
Cite
Cite
Bojana Misheva, Roy Hajjar, Herawaty Sebajang, Frank Schwenter, Minimally invasive management of a paraduodenal hernia with intestinal malrotation, Journal of Surgical Case Reports, Volume 2020, Issue 9, September 2020, rjaa326, https://doi.org/10.1093/jscr/rjaa326
Close - Share Icon Share
Abstract
Paraduodenal hernias (PDHs) are rare entities that may present with acute or subacute symptoms, and which pose challenges to prompt diagnosis and treatment. The minimally invasive management of these hernias is emerging as a new compelling approach to optimize surgical recovery. We present the case of a 42-year-old female patient who presented with acute abdominal pain and symptoms of bowel obstruction. Abdominal imaging suggested the presence of a left PDH. Laparoscopic exploration was performed. Intestinal malrotation was noted with incarceration of a small bowel loop in the Landzert fossa. The incarcerated bowel loop was freed and primary repair of the hernial defect was performed. PDHs are usually congenital and involve a herniation of abdominal content into the left mesocolon, between the mesocolon and the posterior abdominal wall. Minimally invasive treatment, consisting of adhesiolysis and repair of the hernial defect, seems to be a valid and safe option.
INTRODUCTION
Internal hernias account for <1% of cases of intestinal obstruction [1]. Although rare, paraduodenal hernias (PDHs) are the most common type of internal hernias, accounting for half of the cases [2]. Patients with PDH may present with signs or symptoms of acute or chronic bowel obstruction [1]. PDH is classified into left-sided, which account for 75% of the cases, and right-sided, which are less common [3]. Advances in surgical technique have permitted a shift from open to laparoscopic interventions. We describe the successful laparoscopic repair of a left PDH in an adult patient.
CASE PRESENTATION
A 42-year-old female patient presented to the emergency room with acute epigastric pain, nausea and vomiting. Past medical history included hypertension and gastroesophageal reflux disease. Her past medical history did not include any prior abdominal surgery. Vital signs were normal at presentation. Abdominal examination revealed a soft abdomen with a mild epigastric tenderness. White blood cell count and lactate level were within normal limits. An abdominopelvic computed tomography (CT) scan showed a left PDH containing a jejunal loop (Fig. 1). The neck of the hernia was estimated at 4 cm. The bowel had signs of fecalization, suggesting a chronic stasis phenomenon. There was no evidence of occlusion or bowel ischemia.
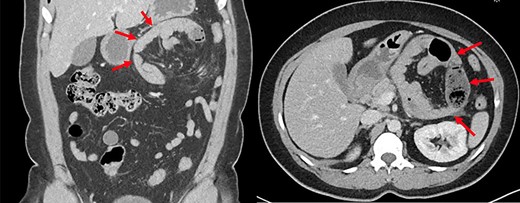
Abdominopelvic CT scan depicting a left paraduodenal hernia containing a jejunal loop with fecalization (arrows).
The patient underwent an exploratory laparoscopy and intestinal malrotation with an internal hernia containing small bowel loops was objectified in the Landzert fossa. The hernia was managed by laparoscopic reduction and closure of the hernial defect. A camera trocar was placed at the umbilical level, two 5 mm trocars were placed in the left iliac fossa and the right hypochondrium, and a 12 mm trocar was placed in the right iliac fossa. The transverse colon and omentum were mobilized to expose the small bowel to the left of the ligament of Treitz. Lysis of adhesions between the transverse mesocolon and the small bowel mesentery allowed access to the hernial sac. Incarcerated small bowel loops were retrieved and were deemed well perfused. The hernial defect was closed with interrupted stitches.
The patient made an uneventful recovery and was discharged at postoperative Day 3. An abdominopelvic CT scan was performed after 3 months and no significant abnormalities were noted. The patient remains well apart from occasional epigastric discomfort.
DISCUSSION
PDHs are congenital hernias caused by an abnormal embryonic rotation of the midgut before re-entering the abdominal cavity [4]. A left PDH involves the paraduodenal fossa of Landzert, which is located lateral to the fourth segment of the duodenum and posterior to the inferior mesenteric vein and left colic artery [5]. The small bowel herniates into the left mesocolon and is entrapped between the mesocolon and the posterior abdominal wall [6]. In the right PDH, the small bowel becomes trapped behind the right mesocolon and mesentery of the cecum. It herniates posteriorly to the superior mesenteric vessels in the fossa of Waldeyer, and the jejunum becomes trapped in the right upper quadrant [7].
The diagnosis of PDH may be challenging as symptoms and physical findings may be nonspecific. Plain abdominal films obtained during an episode of SBO may show dilated jejunal loops clustered toward the upper abdomen. CT is the gold standard for a fast and accurate preoperative diagnosis. The typical appearance of a left PDH on CT scan may consist of jejunal loops in the left upper quadrant, lateral to the duodenum [5].
Principles of surgical management include lysis of adhesions, reduction of the hernia, resection of the ischemic intestinal segment, if any, and closure of the defect. Both open and laparoscopic methods are feasible, the latter gaining popularity with the advancement of surgical techniques. The first laparoscopic repair was reported by Uematsu et al. [8] in 1998. It is not known whether the choice of suture used for closure of the defect affects the risk of recurrence. Prosthetic material was not employed for defect repair in any of the cases reviewed in the literature with one exception reported by Palanivelu et al. [9] in a patient who developed a recurrence after a previous laparoscopic repair.
CONCLUSION
Internal hernias are a rare cause of intestinal obstruction. Among them, PDHs are the most common. Early diagnosis is essential to prevent further complications. Laparoscopy provides a clear anatomical view of the malrotation to confirm the diagnosis. A minimally invasive approach to repair the defect can be carried out safely in order to enhance recovery and shorten hospital stay.
CONFLICT OF INTEREST STATEMENT
The authors have no conflicts of interest to disclose.
PATIENT CONSENT
The patient has provided written consent for the publication of the present manuscript.
References
- surgical procedures, minimally invasive
- acute abdominal pain
- hernias
- intestinal obstruction
- intestine, small
- laparoscopy
- mesocolon
- surgical procedures, operative
- abdomen
- diagnosis
- malrotation, congenital
- paraduodenal hernias
- abdominal imaging
- adhesiolysis
- posterior abdominal wall
- intestinal entrapment



