-
PDF
- Split View
-
Views
-
Cite
Cite
Carlo Marino, Ignacio Obaid, Gabriela Ochoa, Nicolás Jarufe, Jorge A Martínez, Eduardo Briceño, Severe case of post cholecystectomy vasculobiliary injury successfully treated by right hepatectomy with a jump graft to the remaining left hepatic lobe, Journal of Surgical Case Reports, Volume 2020, Issue 9, September 2020, rjaa319, https://doi.org/10.1093/jscr/rjaa319
Close - Share Icon Share
Abstract
Vasculobiliary injuries (VBI) caused by cholecystectomies are infrequent but extremely serious. We report a case of a severe VBI successfully treated at our center. A 22-year-old woman underwent an open cholecystectomy as treatment for acute cholecystitis and bile duct stones. She was transferred to our center on postoperative Day 4 because of progressive jaundice and encephalopathy. After a proper investigation, we found an extreme VBI with infarction of the right hepatic lobe associated with complete interruption of the portal vein and proper hepatic artery flows and full section of the common hepatic duct. Right hepatectomy with portal—Rex shunt revascularization of the left hepatic lobe and Roux-en-Y hepaticojejunostomy to the left hepatic duct was done. The patient was discharged on the 60th postoperative day.
Discussion: This case shows the successful surgical treatment of a severe cholecystectomy’s VBI, avoiding an emergency liver transplant.
INTRODUCTION
Vasculobiliary injuries (VBI) caused by cholecystectomies are infrequent and may be classified into two types: a common variety where the right hepatic artery and bile duct are injured (90%) and an uncommon variety (extreme VBI) where the VBI includes bile duct and proper hepatic artery, common hepatic artery or portal vein. Extreme VBI are more severe and frequently associated with hepatic infarction, often needing a hepatic resection or liver transplantation, with mortality in up to 50% of the patients [1].
We report a case of a severe VBI in a young woman, successfully treated at our hospital.
CASE REPORT
A 22-year-old woman without prior medical history presented to the emergency department from another hospital, with a 2-week history of abdominal pain, nausea, and vomiting. An abdominal ultrasonography found signs of acute cholecystitis associated with choledocholithiasis.
An open cholecystectomy with bile duct exploration was performed. The surgical report informed a severe inflammatory process surrounding the gallbladder that made problematic the exposure and identification of key anatomical landmarks. Also, significative bleeding from the hepatoduodenal pedicle occurred, requiring several stitches for hemostatic control. The surgical procedure ended without proper identification of the pedicle structures.
On the first postoperative day she was taken to the Intensive Care Unit (ICU) because of loss of consciousness. Laboratory analysis shown: white blood cells 40700/μl, C-reactive protein 18 mg/dl, alanine transaminase 4059 U/l, aspartate transaminase 4899 U/l, alkaline phosphatase 331 U/l, gamma-glutamyl transpeptidase 232 U/l, total bilirubin 9.5 mg/dl, direct bilirubin 7.5 mg/dl and International Normalized Ratio 2.1.
She was referred to our center on postoperative Day 4 due to progressive jaundice and encephalopathy. A triphasic contrast-enhanced abdominal computed tomography (CT) was done revealing a right liver lobe infarct, absence of the right and left hepatic arteries (Fig. 1), presence of an accessory left hepatic artery from the left gastric artery (Fig. 2) and right portal vein thrombosis with extension to the main portal vein (Fig. 3).
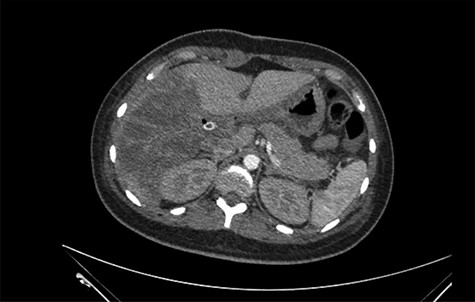
Right liver lobe necrosis and absence of proper hepatic artery on the arterial phase of the triphasic contrast-enhanced abdominal CT.
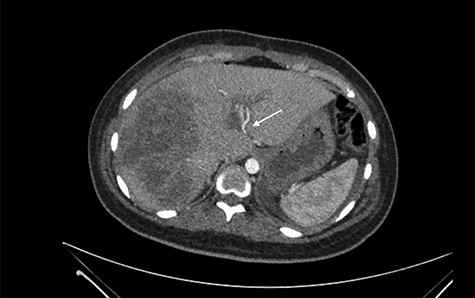
Accessory left hepatic artery (white arrow) on the arterial phase of the triphasic contrast-enhanced abdominal CT.

Main portal vein thrombosis (white arrow) on portal phase of the triphasic contrast-enhanced abdominal CT.
She was taken to the operating room on suspicion of an extreme VBI. Surgical findings were turbid bile peritonitis, right hepatic lobe necrosis and ischemia of the left lobe, complete resection of the common bile duct at the level of the confluence of right and left ducts (Strasberg E3), occlusion of the main portal vein (by several stitches) and a full section of the proper hepatic artery (Figs 4 and 5). The accessory left hepatic artery was not damaged. A right hepatectomy was undertaken. After portal and superior mesenteric vein thrombectomy, revascularization of the left hepatic lobe using a jump-graft (deceased donor iliac vein) from the superior mesenteric vein to the left portal branch at the Rex recessus was done. Also, a Roux-en-Y hepaticojejunostomy to the left hepatic duct was performed (Figs 6–9). Arterial and portal flow was verified with an intraoperative Doppler ultrasound before closure of the laparotomy. After surgery, the patient was shifted to the ICU.
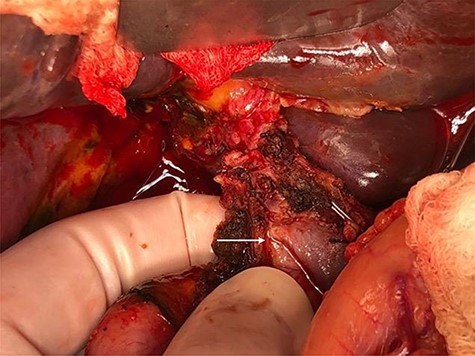
In situ appearance of the hepatic pedicle during exploratory laparotomy. Main portal vein is completely occluded (white arrow).
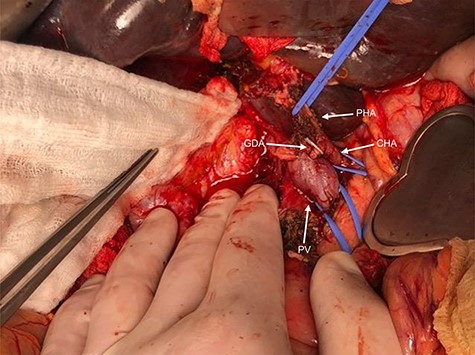
Identification of hepatic pedicle structures. The white arrows show the common hepatic artery (CHA), the completely occluded proper hepatic artery (PHA) and the gastroduodenal artery (GDA) transected for portal vein/superior mesenteric vein (PV) exposure.


Left portal vein at the level of Rex recessus (white arrow). Also, two S4 portal branches are shown (isolated with vascular loops).
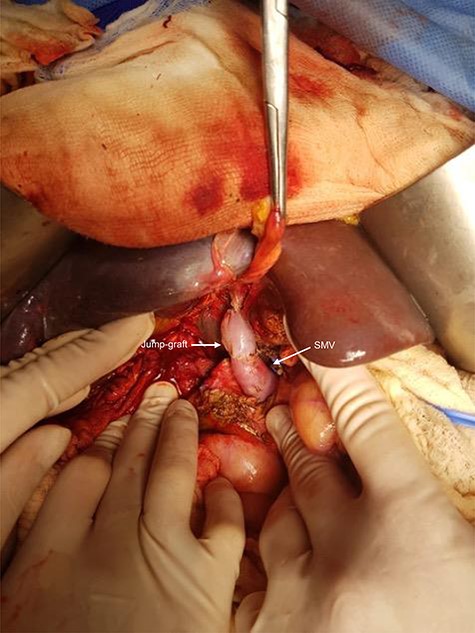
The white arrows show the jump-graft (deceased donor iliac vein) from the superior mesenteric vein (SMV) to the left portal branch at the level of the Rex recessus.

Final image after completion of right hepatectomy and construction of a hepaticojejunostomy to the left bile duct.
Arterial and portal patency was checked by Doppler ultrasound serially after surgery. During evolution, a low-output biliary fistula through the surgical drains was observed associated with an intra-abdominal collection that was treated percutaneously. Additionally, a pleural empyema was diagnosed and treated by thoracoscopic approach.
The patient was discharged on the 60th postoperative day. After 12 months of follow-up the patient remains asymptomatic.
Histopathological analysis of the right liver reported hepatic infarction.
DISCUSSION
Bile duct injuries (BDI) are rare, with incidences in the range 0.15–0.6% [2] and 0.1–0.3% [3] in laparoscopic and open cholecystectomies, respectively. Nevertheless, they are associated with a major impact in quality of life [4] and reduced long-term survival [5] in affected patients.
The focus should be on prevention to minimize the incidence of BDI. Recommendations for reduction of these injuries include correct exposure of Calot’s triangle, achievement of the critical view of safety, partial cholecystectomy in cases of difficult dissection and dome-down cholecystectomy when Calot’s triangle is severely inflamed [6].
Extreme VBI represents approximately 8–10% of VBI [1,7]. Features usually associated with more severe vascular injuries are intense inflammation and contraction of the gallbladder, fundus-down cholecystectomy with no clear dissection plane between gallbladder and liver, and hemorrhage [7]. This case had at least two of those characteristics at index surgery (severe inflammation and bleeding).
According to a literature review of hepatectomies for post-cholecystectomy BDI, 5.6% of patients required a liver resection as treatment, with the majority of them being right lobectomies [8]. Only 10% were urgent hepatectomies (within 2 weeks after initial surgery) and complications rates were high, with biliary fistula occurring in 25–39% of patients. The mortality rate was 11.1%, being significantly higher among those carried out as urgent procedures (3.8% vs 44.4%). In the same study, BDI Strasberg types E4 or E5 and/or concurrent arterial injuries were identified as independent risk factors for hepatectomy.
Liver transplantation (LT) is occasionally the last resource in the treatment of BDI. It could be performed as an emergency procedure in cases of post-injury acute liver failure or as an elective surgery in patients who progress to chronic liver disease [9]. Waiting list mortality in these patients ranges between 7.4 and 20%, depending on each country’s donation rates [9,10]. In a Latin American series, complications and mortality rates among these patients were 56.2 and 12.5%, respectively [10].
This case report presents the successful treatment of a young woman with an extreme VBI after an open cholecystectomy. The presence of an accessory left hepatic artery probably favored that the patient did not remain anhepatic after index surgery. Maintained arterial perfusion in the lateral sector of the liver with a minimum of liver function, ultimately allowed her survival for a few days before performing the portal revascularization of the left lobe. Likewise, this accessory artery avoided intrahepatic biliary ischemia of the lateral segments, reducing the possibility of developing future ischemic cholangiopathy.
To the best of our knowledge, this would be the first report on rescue of liver function in a patient with a VBI using a hepatectomy and a meso-Rex shunt, avoiding an emergency liver transplant.
CONFLICT OF INTEREST STATEMENT
None declared.
References
- cholecystitis, acute
- cholecystectomy
- hepatic resection
- hepatic artery
- common hepatic duct
- infarction
- jaundice
- liver transplantation
- portal vein
- surgical procedures, operative
- tissue transplants
- encephalopathy
- bile duct calculi
- revascularization
- cholecystectomy, open
- left hepatic duct
- liver lobe
- roux-en-y hepaticojejunostomy
- mesoportal shunt



