-
PDF
- Split View
-
Views
-
Cite
Cite
Siang Wei Gan, Martin Bruening, Shantanu Bhattacharjya, Hybrid laparoscopic and open repair of post-nephrectomy flank hernia, Journal of Surgical Case Reports, Volume 2020, Issue 9, September 2020, rjaa299, https://doi.org/10.1093/jscr/rjaa299
Close - Share Icon Share
Abstract
Surgical repair of flank hernia is not routinely performed, due to perceived technical difficulties with the surgery and risk of recurrence, or the misconception that flank hernia is solely due to a denervation injury. Due to the rareness of flank hernia in the literature, there is no general consensus on the best method of surgical repair. We present the case of a patient with a symptomatic large flank hernia following open nephrectomy, in which a hybrid technique of open and laparoscopic flank hernia repair with sublay mesh and bone anchor fixation was successfully performed with good outcome. This case highlights the benefits of the hybrid approach, which allowed a laparoscopic assessment of the defect and adhesiolysis, followed by the open repair which enabled adequate mesh overlap, fixation to surrounding tissues and bone anchor fixation.
INTRODUCTION
Flank hernia, which is usually iatrogenic following surgical access or traumatic in origin, is a relatively rare presentation compared with other types of hernia. Surgical repair is complex due to its location and close proximity with other structures, making mesh overlap and fixation difficult. As flank hernias are an infrequent topic of discussion in the literature, there is no general consensus regarding the best method of repair, and no significant prospective trials [1].
CASE REPORT
A 60-year-old lady developed right flank bulge shortly after open nephrectomy for a chronically infected right kidney due to renal calculi. The bulge had been managed conservatively due to perceived technical difficulties and high risk of failure with flank hernia repair. In addition, there was a component of postdenervation myopathy. Surgery was considered in light of worsening pain, inability to perform daily activities and increasing size of the bulge. Significant medical history included morbid obesity (BMI > 35) and previous open cholecystectomy through a Kochers incision. On examination, she had a large non-tender right flank bulge (Fig. 1) with unconfirmed reducibility. Computed tomography revealed a large necked right abdominal wall hernia containing multiple loops of small bowel, hepatic flexure, distal appendix, fat and lateral right lobe of the liver.

After evaluation, she underwent a hybrid laparoscopic and open incisional flank hernia repair with concomitant limited flank abdominoplasty. The hernia was marked to delineate skin flap limits for abdominoplasty. A diagnostic laparoscopy was performed (Fig. 2a). The hernia defect extended from the right subcostal region to the right iliac crest, medially close to the midline and posteriorly up to the lumbar muscles. Laparoscopic adhesiolysis was performed and hernia sac reduced. The previous nephrectomy scar and large redundant abdominal lateral wall (25 × 15 cm) were excised. The plane between residual external and internal oblique muscles and the transverse abdominis muscle was identified and developed. The fascia transversalis and transversus abdominis muscles were plicated together to create a new preperitoneal layer. A large 30 × 30 cm Ultrapro (Ethicon) mesh was placed in this interstitial position and secured with 2–0 polydioxanone sutures (PDS) and fixed with ProTack (Covidien) fixation device to the lower ribs and iliac crest (Fig. 2b). The external and internal oblique muscle flaps were approximated with 2–0 PDS and a further 10 × 15 cm Ultrapro mesh was placed onlay covering the medial aspect of the defect and secured with ProTack and PDS sutures. Two 15Fr Blake drains were placed in under fat plane. Scarpa fascia was sutured with 2–0 Vicryl. Skin closed with staples and 3–0 Nylon sutures (Fig. 3a). Abdominal binder was used over the dressing.
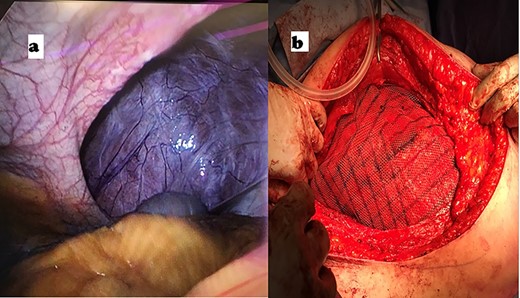
(a) Laparoscopic intraperitoneal view of abdominal defect; (b) placement of large Ultrapro mesh in sublay position.
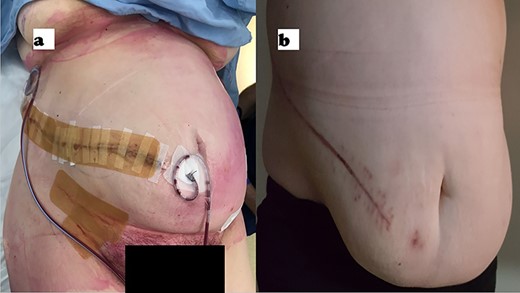
Postoperative photograph of the wound on day of surgery (a) and at 24 weeks (b).
Clinical recovery was uneventful. One drain was removed prior to discharge on the fourth postoperative day, and the other on day 9 while draining 44 ml over 24 h. She had a good result postoperatively with resolution of the bulge and preoperative symptoms. There was no evidence of recurrence at 6 months’ follow-up (Fig. 3b).
DISCUSSION
Flank hernia is a relatively rare entity with only about 350 known cases published previously [2]. It is defined as a hernia occurring lateral to the rectus muscle sheath, and within 3 cm above and below the umbilicus [3]. Most are incisional hernias from previous surgery for urologic procedures, aortic repair or iliac bone harvesting [4], and a smaller number are traumatic or congenital in origin. Flank incisional hernia occurs in ~17% of patients after nephrectomy or aortic repair [2].
Surgical repair is technically challenging with limited space for mesh placement and fixation due to the close proximity to neurovascular and bony structures [5]. Lack of familiarity among surgeons, difficulty determining extent of defect and weakness of surrounding tissues are other issues complicating repair [6]. In addition, there may be a flank bulge from concomitant abdominal muscle denervation from 11th and 12th thoracic nerve injury from the prior flank incision, which can persist postoperatively despite a successful hernia repair [4].
A variety of approaches to repair flank hernias have been reported, including open through the previous flank incision, midline or abdominoplasty [7, 8]; laparoscopic [6], or a combination of both [4, 9]. Laparoscopic repair is usually limited to smaller defects. The mesh, while always used, is usually placed sublay, and onlay or intraperitoneal onlay mesh is used when the retromuscular space is insufficient [2].
Our hybrid approach enabled us to capitalize on the benefits of both laparoscopic and open surgery. The initial diagnostic laparoscopy enabled thorough assessment of the defect extent, laparoscopic adhesiolysis and safe reduction of the hernia sac. The subsequent open approach allowed us to ensure adequate overlap of the mesh and surrounding tissues, and perform bony fixation of the mesh to the lower ribs and iliac crest. The mesh was placed sublay in keeping with the mesh position most commonly reported [5, 10].
In conclusion, the hybrid laparoscopic and open technique is feasible for large incisional flank hernia repair with good outcomes. The patient denied chronic pain or hernia recurrence at 6 months and reported high satisfaction with the surgery.
CONFLICT OF INTEREST STATEMENT
None declared.



