-
PDF
- Split View
-
Views
-
Cite
Cite
Kevin Corless, Amir Samy, Ahmed Kamil, Aisling Maria Hogan, Benign cyst with xanthogranulomatous inflammation involving the transverse colon and the common iliac artery, Journal of Surgical Case Reports, Volume 2020, Issue 9, September 2020, rjaa295, https://doi.org/10.1093/jscr/rjaa295
Close - Share Icon Share
Abstract
Xanthogranulomatous inflammation (XGI) is a rare process. Colonic XGI is extremely rare. We present a case report of XGI arising within an intra-abdominal cyst involving the transverse colon. A 28-year-old man presented with abdominal discomfort. He underwent a computed tomography abdomen–pelvis, which found three subcutaneous collections and a large cystic intra-abdominal structure. The decision was made for resection. Intraoperatively, the cyst originated from the pelvis and was adherent to the surrounding tissues. Histology from the lesion revealed XGI extending into the surrounding tissue. XGI is a rare inflammatory condition. Clinically, it can be difficult to distinguish XGI from an infiltrative malignancy. Therefore, it is usually necessary to obtain a pathological diagnosis of XGI. This case describes an atypical cystic lesion with XGI involving the transverse colon. Although rare, it should be considered in the potential differential diagnosis of an infective or malignant mesenteric cyst.
INTRODUCTION
Xanthogranulomatous inflammation (XGI) is a rare chronic inflammatory process characterized by aggregation of lipid-laden foamy macrophages or xanthoma cells [1]. XGI can involve any organ, most commonly kidneys and gallbladder [2, 3]. Colonic XGI is extremely rare as there are <10 reported cases in the literature. XGI presents as a mass-like lesion, with predominant submucosal involvement. Clinically, XGI is difficult to differentiate from infiltrative cancer as it usually presents as an irregular mass-like lesion, with extensive fibrosis and inflammation [4].
We present a case report of XGI arising within an intra-abdominal cyst involving the transverse colon and encasing the common iliac artery.
CASE REPORT
A 28-year-old man presented to the plastic surgery service with a suspected intra-abdominal collection 10 days after liposuction performed abroad. He had recently undergone 20 kg weight loss and weighed 63 kg. He presented with a history of increasing abdominal discomfort, nausea, fevers and chills.
He had no history of any previous intra-abdominal pathology or surgery. He had no significant medical co-morbidities.
He became increasingly unwell with sepsis secondary to the abdominal collection. Vital signs demonstrated a pyrexia of 38.5°C, heart rate 104 bpm, blood pressure 137/86 and respiratory rate 20. On examination, there was minimal abdominal adiposity, but his peritoneal cavity was distended by a huge fluctuant mass. There was generalized tenderness and maximal guarding within the left iliac fossa.
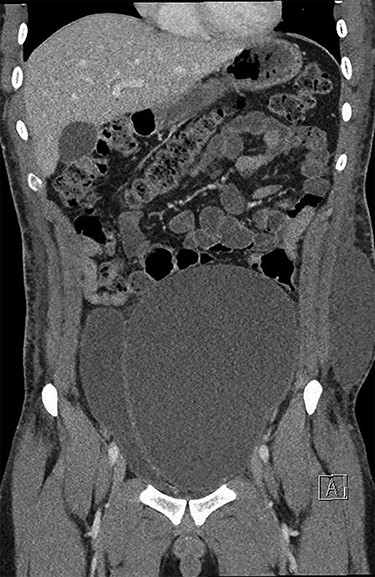
He underwent a computed tomography (CT) abdomen and pelvis, which demonstrated three subcutaneous cystic collections in the left flank, right flank and the left rectus abdominal muscle measuring 12.5 × 3.5 × 10.7, 5.9 × 1.2 × 7 and 1.2 × 1.8 × 2 cm. A large cystic intra-abdominal structure displaced the bladder to the right side and measured 18 × 14 x 7.6 cm (Figs 1 and 2).

The decision was made at this point to treat the patient’s underlying sepsis prior to any intervention of the intra-abdominal masses. He was treated with broad-spectrum intravenous antibiotics and subcutaneous drainage of the infective collections. He was discharged home for preoperative evaluation and optimization prior to surgical intervention for the lesion.
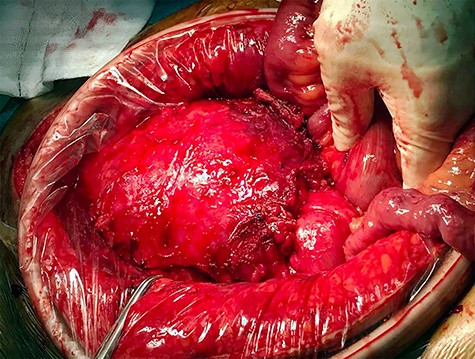
The case was discussed at a Gastrointestinal Multidisciplinary meeting and the decision was made for surgical resection of the intra-abdominal lesion via a midline laparotomy. At laparotomy, the cyst was originating from the pelvis and adherent to pubic symphysis, transverse colon and common iliac vein (Fig. 3). The cyst was mostly resected via an en bloc distal transverse colectomy with the cyst leaving right colon and hepatic flexure in situ; however, < 5% was left in place as it was adherent to the common iliac vein and could not be safely resected without risk of significant bleeding.
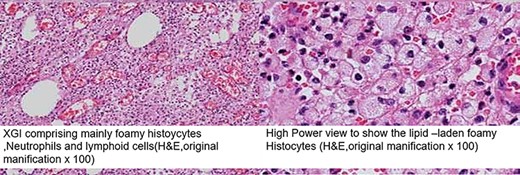
He had an excellent post-operative course and was discharged home Day 9 post-operatively. Histological examination demonstrated a fibrotic, thickened cyst wall lined by granulation tissue with active inflammation and haemosiderin deposition with marked XGI within the cyst wall extending into the surrounding adipose tissue and a portion of the transverse colon with no evidence of ischaemia. Samples of the cyst contents were sent to microbiology showing no evidence of any microorganism growth on culture or molecular testing and had negative Ziehl–Nielsen staining. There was no evidence of dysplasia or malignancy (Fig. 4).
He has subsequently undergone reversal of colostomy and remains well. Follow-up axial imaging does not demonstrate any residual or recurrent disease.
DISCUSSION
XGI is a rare chronic inflammatory condition characterized by clustering of foamy macrophages amongst other inflammatory cells [1], most typically found in the gallbladder and the kidney [2, 3]. It has been described in a variety of other locations including the respiratory tract, the male and female reproductive tracts, the gastrointestinal tract and others. XGI involving the lower GI tract is rare, with eight cases having previously been described in the literature, but none describing involvement of the transverse colon (Table 1).
| Author . | Age/Sex . | Symptoms . | Primary focus . | Secondary focus . |
|---|---|---|---|---|
| Lo et al. [5] | 72/M | Constipation, abdominal pain | Sigmoid colon | Sigmoid colon |
| Oh et al. [6] | 38/F | Abdominal pain, fever, diarrhoea | Sigmoid colon | Sigmoid colon, appendix, salpinx |
| Anadol et al. [7] | 57/F | Fatigue, abdominal pain, PR bleeding | Caecum | Caecum, appendix |
| Dhawan et al. [8] | 60/M | abdominal pain, vomiting, constipation | Ascending colon | Ascending colon |
| Chieco et al. [9] | 56/F | Abdominal pain, weight loss, fever | Caecum | Caecum, ileocaecal valve |
| Chon and Kim [10] | 34/F | Abdominal pain | Terminal ileum | Terminal ileum |
| Author . | Age/Sex . | Symptoms . | Primary focus . | Secondary focus . |
|---|---|---|---|---|
| Lo et al. [5] | 72/M | Constipation, abdominal pain | Sigmoid colon | Sigmoid colon |
| Oh et al. [6] | 38/F | Abdominal pain, fever, diarrhoea | Sigmoid colon | Sigmoid colon, appendix, salpinx |
| Anadol et al. [7] | 57/F | Fatigue, abdominal pain, PR bleeding | Caecum | Caecum, appendix |
| Dhawan et al. [8] | 60/M | abdominal pain, vomiting, constipation | Ascending colon | Ascending colon |
| Chieco et al. [9] | 56/F | Abdominal pain, weight loss, fever | Caecum | Caecum, ileocaecal valve |
| Chon and Kim [10] | 34/F | Abdominal pain | Terminal ileum | Terminal ileum |
M, male; F, female.
| Author . | Age/Sex . | Symptoms . | Primary focus . | Secondary focus . |
|---|---|---|---|---|
| Lo et al. [5] | 72/M | Constipation, abdominal pain | Sigmoid colon | Sigmoid colon |
| Oh et al. [6] | 38/F | Abdominal pain, fever, diarrhoea | Sigmoid colon | Sigmoid colon, appendix, salpinx |
| Anadol et al. [7] | 57/F | Fatigue, abdominal pain, PR bleeding | Caecum | Caecum, appendix |
| Dhawan et al. [8] | 60/M | abdominal pain, vomiting, constipation | Ascending colon | Ascending colon |
| Chieco et al. [9] | 56/F | Abdominal pain, weight loss, fever | Caecum | Caecum, ileocaecal valve |
| Chon and Kim [10] | 34/F | Abdominal pain | Terminal ileum | Terminal ileum |
| Author . | Age/Sex . | Symptoms . | Primary focus . | Secondary focus . |
|---|---|---|---|---|
| Lo et al. [5] | 72/M | Constipation, abdominal pain | Sigmoid colon | Sigmoid colon |
| Oh et al. [6] | 38/F | Abdominal pain, fever, diarrhoea | Sigmoid colon | Sigmoid colon, appendix, salpinx |
| Anadol et al. [7] | 57/F | Fatigue, abdominal pain, PR bleeding | Caecum | Caecum, appendix |
| Dhawan et al. [8] | 60/M | abdominal pain, vomiting, constipation | Ascending colon | Ascending colon |
| Chieco et al. [9] | 56/F | Abdominal pain, weight loss, fever | Caecum | Caecum, ileocaecal valve |
| Chon and Kim [10] | 34/F | Abdominal pain | Terminal ileum | Terminal ileum |
M, male; F, female.
The exact pathogenesis underlying the condition is not well described. Proposed hypotheses include defective lipid transport, immunological disorders such as disturbed chemotaxis of polymorphonuclear cells and macrophages, a specific immune response towards Proteus and Escherichia infections, and lymphatic obstruction [3].
Clinically, it can be difficult to distinguish XGI from an infiltrative malignancy due to the appearance of the lesion, with typically an irregular mass-like lesion with extension of fibrosis and inflammation into the surrounding normal tissues. Therefore, it is usually necessary to obtain a pathological diagnosis of XGI. In our case, the diagnosis was revealed after an exploratory laparotomy was performed for removal of the cystic lesion. It was also found that the lesion was adherent to several surrounding structures including the common iliac vein and the transverse colon, necessitating a partial colectomy and a remnant of the cystic lesion had to be left in situ for operative safety.
This case describes the atypical finding of a cystic lesion with XGI involving the transverse colon and the common iliac vein. Although a rare pathology, it should be considered in the potential differential diagnosis of an infective, malignant or mesenteric cyst.
CONFLICT OF INTEREST STATEMENT
None declared.



