-
PDF
- Split View
-
Views
-
Cite
Cite
Rony Shah, Linda Klumpp, Juan Negron-Diaz, Torr Carmain, Jeffrey Jordan, HCA Healthcare/USF Morsani College of Medicine GME Programs at Citrus Memorial Hospital, Inverness, Florida, Transverse colon volvulus in a patient with autism, Journal of Surgical Case Reports, Volume 2020, Issue 9, September 2020, rjaa284, https://doi.org/10.1093/jscr/rjaa284
Close - Share Icon Share
Abstract
Transverse colon volvulus is an extremely rare cause of bowel obstruction with approximately 100 cases reported in literature. Transverse colon volvulus presents with signs and symptoms of large bowel obstruction, but it can become a surgical emergency due to bowel infarction or peritonitis. We present a rare case of transverse colon volvulus in a 36-year-old male patient with severe autism. We hope this case report will raise awareness of this disease.
INTRODUCTION
Transverse colon volvulus is an extremely rare cause of bowel obstruction; it constitutes approximately 5% of all causes of bowel obstruction [1]. There have been ~100 total cases reported in literature [2]. Transverse colon volvulus presents with signs and symptoms of large bowel obstruction, but it can become a surgical emergency due to bowel infarction or peritonitis [1–2]. This disease has a high risk of mortality, so it requires urgent diagnosis and surgical intervention. We present a rare case of transverse colon volvulus in a patient with severe autism.
CASE PRESENTATION
A 36-year-old male presented to the emergency room (ER) for not having a bowel movement, abdominal distension, decreased appetite and increased lethargy for 3 days. Patient is nonverbal, so majority of the history was obtained from his caretaker. He reported a past medical history of severe autism. Vitals were temperature 98.8 F, blood pressure 127/88 mmHg, heart rate 125 beats per minute, respiratory rate 24 breaths per minute and oxygen saturation 94%. On physical examination patient appeared somnolent with a distended abdomen, decreased bowel sounds and mild diffuse tenderness on palpation. Laboratory results were significant for white blood count (WBC) 25.8 U/L, hemoglobin (Hg) 12.3 g/dL, platelet 370 × 103 U/L, blood urea nitrogen (BUN)/creatinine 14/0.5 mg/dL, aspartate aminotransferase (AST) 13 U/L, alanine aminotransferase (ALT) 12 U/L, alkaline phosphatase 121 U/L, lipase 25 U/L and lactic acid 4.64 mmol/L. Computed tomography (CT) scan demonstrated marked distension of the cecum and a colonic loop in the right upper abdomen due to a volvulus possibly in the ascending colon and is unable to visualize the transverse and proximal descending colon and a foreign body within the stomach (Fig 1A–C). Patient was taken for an emergent exploratory laparotomy; however prior to the procedure, he underwent an esophagogastroduodenoscopy (EGD). A foreign body was found in the stomach, but it was too large to be extracted on EGD. Examination of the abdominal cavity intraoperatively revealed a dilated colon (15 cm), a large section of volvulized colon in the right upper quadrant and a segment of volvulus in the distal transverse colon. Patient underwent an extended right hemicolectomy with anastomosis of the terminal ileum to the transverse colon at the level of the splenic flexure. He also underwent a gastrotomy to remove the foreign body, which appeared to be rolled up tar paper. He was started on empiric antibiotic regimen of vancomycin, ciprofloxacin and metronidazole for 2 days. His antibiotics were de-escalated to ceftriaxone and metronidazole and continued for an additional 5 days. Patient had a nasogastric tube placed following the procedure which continued to drain bilious material for 3 days before it was removed. His diet was advanced as tolerated. He was safely discharged to his group home, and no complications were noted at patient’s 2-week follow-up with general surgery.
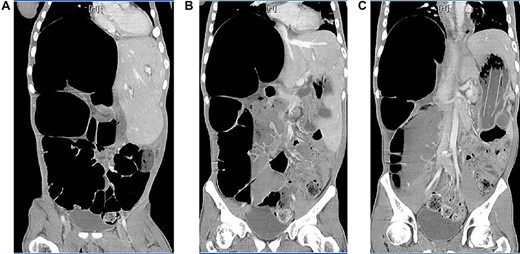
Axial view of CT of abdomen and pelvis with intravenous contrast (A) & (B), dilated cecum and colonic loop in the right upper quadrant and (C) foreign body within the stomach.
DISCUSSION
Majority of the volvulus occur in the sigmoid colon (60–80%), cecum (20–40%) and transverse colon (3%) [1, 3]. The mortality rate of transverse colon volvulus is 33% compared to 21% for sigmoid colon volvulus and 10% for cecum volvulus [1–2]. Any segment of the colon can get rotated if it has a long loose mesentery which becomes narrow at the base [2, 4]. This is less likely to occur in the transverse colon due to its short mesentery and fixed hepatic and splenic flexure [1, 2]. Several predisposing risk factors are history of volvulus, previous surgery involving bowel translocation, malignancy, distal colonic obstruction, adhesions and congenital defects such as intestinal malrotation with an inadequate fixation of posterior abdominal wall, chilaiditis syndrome, Clostridium difficile-associated pseudomembranous colitis, pregnancy and chronic constipation because it causes severe elongation of the transverse colon [1–2, 5–10]. In our case patient’s mental status and the foreign body within his stomach may have contributed to chronic constipation as a risk factor for his transverse colon volvulus. The two most common presentations of transverse colon volvulus are acute fulminating type and subacute progressive type. The acute fulminating type presents with sudden onset of severe abdominal pain, rebound tenderness, nausea, vomiting, mild abdominal distension, severe leukocytosis and clinical deterioration [1–2, 5]. The subacute progressive type presents with mild abdominal pain, severe abdominal distension, normal to mildly elevated leukocytosis and clinically stable [1–2, 5]. Our patient’s mental status made it difficult to clinically evaluate him, but his physical exam findings and laboratory findings suggest that he had the subacute progressive type which was progressing to the acute fulminating type. Early diagnosis of the subacute progressive type can be challenging which allows it to progress to the life-threatening acute fulminant type with bowel infarction, peritonitis and death [5 and 6]. The diagnosis of transverse colon volvulus is typically made intraoperatively because the radiographic findings are not as characteristic as seen in sigmoid colon volvulus [1–2, 5]. There are no typical radiographic findings of transverse colon volvulus seen on a CT [5]. The classical ‘bird’s beak’ appearance of the transverse colon is seen with contrast enema, but it is not recommended in acute settings because it can delay surgical intervention [1–2, 5]. The CT scan findings in our case suggested a volvulus, but we were unable to identify the exact location of the volvulus. The treatment is not decompression as it is in cecal or sigmoid volvulus due to the risk of failure and necrosis [1–2, 5]. Treatment options include detorsion of the bowel, untwisting with colopexy, surgical resection with primary anastomosis or surgical resection with stoma formation [1–2, 5]. Surgical resection with primary anastomosis or stoma formation is the preferred option because it prevents recurrence [1–2, 5–6, 9]. Simple detorsion of the bowel and untwisting with colopexy are not the preferred treatment options due to the higher risk of recurrence or even death [1–2, 5, 7, 9]. Our patient underwent surgical resection with primary anastomosis.
CONCLUSION
Transverse colon volvulus is a rare cause of large bowel obstruction with an extremely high mortality rate. Early diagnosis and treatment can reduce the risk of mortality as seen in our patient. We hope our case report will raise awareness of this disease.
DISCLAIMER
This research was supported in part by HCA Healthcare and/or an HCA Healthcare-affiliated entity. The views expressed in this publication represent those of the author(s) and do not necessarily represent the official views of HCA Healthcare or any of its affiliated entities.
CONSENT
The patient provided informed consent.
Conflict of Interest
No conflict of interest to report.
FUNDING
None.



