-
PDF
- Split View
-
Views
-
Cite
Cite
Idrees Ahmed, James Murray, Dislocation of a polyethylene insert in an infected knee joint after a Triathlon total knee arthroplasty, Journal of Surgical Case Reports, Volume 2020, Issue 8, August 2020, rjaa287, https://doi.org/10.1093/jscr/rjaa287
Close - Share Icon Share
Abstract
This report presents the case of a 57-year-old male patient who underwent a total knee arthroplasty (TKA) using an uncemented Triathlon system and subsequently went on to develop a prosthetic joint infection (PJI) with eventual polyethylene insert dislocation. This report presents the clinical, radiological and surgical findings of the insert dislocation on the background of PJI and explores this rare complication of TKA by providing a summary of the literature on this topic.
INTRODUCTION
This paper presents the case of a dislocated polyethylene insert (DPI) in a Triathlon® (Stryker Orthopaedics, UK) total knee arthroplasty (TKA). There have only been a handful of papers published in the wider literature regarding DPIs in TKA [1–8]. However, to our knowledge there are no reported cases of polyethylene insert dislocation secondary to prosthetic joint infection (PJI) as is reported in this case.
This report aims to provide a literature review of DPI in TKA with a focus on the clinical presentation and the proposed mechanism of insert dislocation. Similarities and differences between our case and the literature are highlighted.
CASE PRESENTATION
A 57-year-old male patient received an uncemented TKA for persistent symptoms of arthritis. The patient was discharged 3 days post operation; however, re-presented with symptoms of swelling of the right knee, pyrexia wound exudate and decreased range of motion (ROM).
Blood cultures grew Staphylococcus aureus and a PJI was diagnosed.
The debridement, antibiotics and implant retention (DAIR) procedure was completed with exchange of the modular Triathlon polyethylene insert.
During the procedure it was noted that there was pus in the joint. Post DAIR the patient was placed on antibiotics and received regular outpatient review.
During outpatient review, ROM of the right knee had improved and radiographs taken revealed a well-fixed and located joint prosthesis. However, 6 days after stopping antibiotics the patient presented to hospital with a swollen right knee and pyrexia. Clinical examination of the right knee joint revealed reduced ROM and anteroposterior instability of the joint. Subsequent imaging showed a dislocated Triathlon polyethylene insert.
Given that previous attempts to treat the PJI with implant retention had failed, the patient underwent a first-stage revision TKR Triathlon to Heraeus medium spacer with Copal® Gentamycin + Clindamycin (Heraeus Medical). During the operation it was noted that there was the presence of biofilm membrane beneath the liner and fibrous tissue in the joint (Fig. 1).
The growth of fibrous tissue appeared to have infiltrated key components of the Triathlon implant, notably between the tibial baseplate and where the dislocated liner sat (Fig. 2).
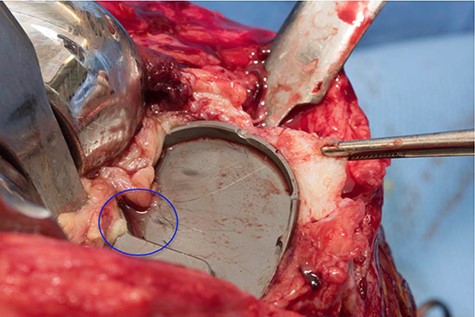
Intraoperative photograph showing the presence of biofilm on the tibial component (blue circle), note the presence of retracted fibrous tissue.
Postoperatively the patient was commenced on a further course of antibiotics and is scheduled for a second-stage revision to a definitive prosthesis at 6 months after explantation.
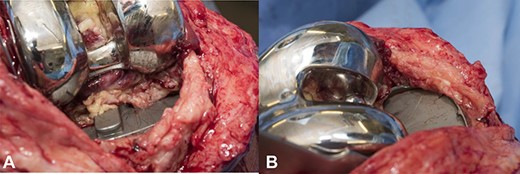
(a) Fibrous tissue growth in the posterior aspect of the right knee joint, (b) fibrous tissue growth in the anteromedial aspect of the right knee joint.
DISCUSSION
The patient presented with symptoms of swelling, reduced ROM and instability, which are symptoms previously reported for DPIs [2, 4, 5, 7]. Other symptoms of DPI that have been reported include the sensation of popping/clicking within the knee joint on movement and joint locking [2–4, 7].
DPI in TKA can not only cause a TKA to fail but also cause damage to the surrounding structures such as the lateral retinaculum and patella tendon by direct trauma and metallosis of synovial tissue [1, 5]. The variability of presenting symptoms combined with the fact that DPI is a rare complication of TKA can make it challenging to diagnose [1].
Previously reported cases of DPI have occurred in the absence of systemic or local infection. To the authors’ knowledge no previously reported cases of DPI have occurred on a background of PJI. The significance of this from a diagnostic point of view is that the added pathology of PJI can present with symptoms that are similar to that of DPI, for example, joint pain, effusion and signs of potential implant loosening [9]. Therefore, there is a risk that after treating the PJI any DPI may be missed for a prolonged period of time if not initially picked up on radiographs.
Reported cases of DPI in TKA have been atraumatic in nature with only one paper commenting on a traumatic mechanism of insert dislocation [5]. In nearly all reported cases no clear cause for dislocation was identified; however, authors have proposed mechanisms as to how dislocation may have occurred. The most popular proposed mechanism of dislocation is that repeated posteriorly directed compressive force on the polyethylene insert from the femur results in anterior lift off of the insert and subsequent dislocation [3–5, 8]. Davis et al. [8] gave a biomechanical basis for this theory stating that during knee flexion femoral tibial contact moves posteriorly leading to anterior lift off of the insert. Anterior lift off of the insert may be possible due to either failure to secure the insert at surgery, overt locking mechanism failure or repeated stress causing wear on the locking mechanism and eventual failure [8]. Poulter and Ashworth [7] describe a case of insert dislocation thought to be caused by uneven distribution of load on the insert. The authors postulated that ligament laxity in their patient’s knee led to point bearing of the lateral femoral condyle onto the posterolateral corner of the polyethylene insert leading to accelerated wear and failure of the inserts retaining lip leading to dislocation. Rutten and Janssen [2] proposed that impingement of the insert on soft tissues or osseous structures can lead to a DPI. The authors hypothesized this after finding a large posterior osteophyte in their patient who had a DPI and believed that this structure was responsible for the dislocation [2].
The patient reported on in this paper had satisfactory alignment and a well-fixed prosthesis prior to experiencing insert dislocation. Given the excellent range of movement following TKA, this makes incorrect initial placement of the components and insert during surgery unlikely. In addition, there were no findings of ligament laxity, making any load distribution issues and subsequent accelerated wear and failure of the insert also unlikely. With the history of PJI and the growth and infiltration of fibrous tissue in between the insert and tibial component of the TKA (Fig. 2), one can postulate that the disruption to the insert by the fibrous tissue may have contributed to its eventual dislocation.
By presenting this case report it is hoped that there will be increased awareness of the occurrence of DPIs as a complication of TKA, leading to improved recognition, timely diagnosis and reduced complications of insert dislocation. In addition, specific to this case is that DPI may be caused by joint infection, something that has not been previously reported in the literature.
ACKNOWLEDGEMENTS
The authors thank Mr J.M. for contributing to the writing and proof reading of the manuscript.
CONFLICT OF INTEREST
None declared.
FUNDING
None.



