-
PDF
- Split View
-
Views
-
Cite
Cite
Amjad Soltany, Ghazal Asaad, Rami Daher, Mouhannad Dayoub, Ali Khalil, Zuheir Alshehabi, A maxillary ameloblastic fibrosarcoma tumor: a rare case report from Syria, Journal of Surgical Case Reports, Volume 2020, Issue 8, August 2020, rjaa255, https://doi.org/10.1093/jscr/rjaa255
Close - Share Icon Share
Abstract
Ameloblastic fibrosarcoma (AFS) is a rare, aggressive malignant odontogenic tumor. AFS is seen most frequently in second and third decades of life. We are reporting a case of a low grade AFS in a 21-year-old male complaining of a painless swelling in the right side of the maxilla. The patient was treated with surgical excision followed by radiotherapy, which is considered the most effective approach for most of soft tissue sarcomas. AFS has a high-reported recurrence rate (up to 37%); therefore, long-term surveillance for recurrence is crucial.
INTRODUCTION
Ameloblastic fibrosarcoma (AFS) is a rare malignant odontogenic tumor composed of benign epithelium and malignant mesenchyma [1, 2]. It could originate from ameloblastic fibroma (AF) (two-third of the reported AFS cases) or as a malignant tumor (de novo) (one-third of the reported AFS cases). Like the majority of soft tissue sarcoma cases, the etiology of this tumor is still unknown [3].
AFS is most likely seen in second and third decades of life with a wide range (3–89 years). It is distributed equally in both sexes with a slight larger percentage in males [2, 4]. Usually, the mandible is the most affected site; however, in this case, the tumor was found in the maxilla [2]. The treatment of AF usually involves surgical excision with removal of the affected teeth. But in cases of AFS, chemotherapy and radiotherapy could be used as adjuvant therapies although chemotherapy has not been determined clearly in the treatment guideline for AFS [5]. On the other side, the combination of doxorubicin and olaratumab has been permitted as a first-line therapy for patients with advanced soft-tissue sarcoma responding to anthracycline therapy [6]. Recurrence rate of AFS ranges from about 24% to 37% with a reported incidence of distant metastases of 4.5%; therefore, long-term follow-up is crucial [5].

Clinical appearance of the tumor at the time of diagnosis, showing a swelling in the palatine process of maxilla, spreading from the vestibule of the mouth reaching the upper right premolars.
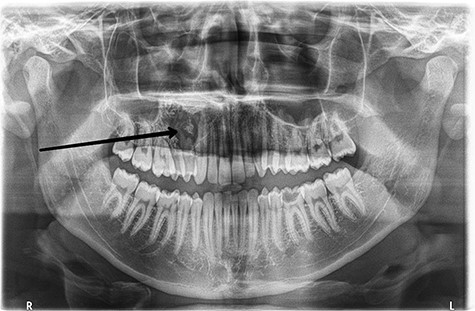
Preoperative orthopantomogram shows the radiolucent area with the calcified lesions in the right hemi-maxilla with resorption in the roots of the upper right premolars.
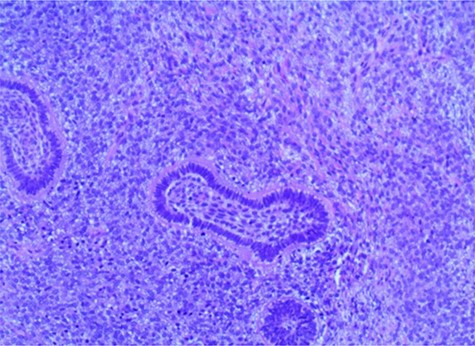
Biphasic tumor composed of islands of benign odontogenic epithelium and an abundant malignant mesenchymal component consisted of ovoid and fusiform cells, in addition to plump and spindle stromal cells that show hyper-cellularity and nuclear polymorphisms associated with cytologic atypia, mitotic figures and anaplasia (hematoxylin-eosin, x40).
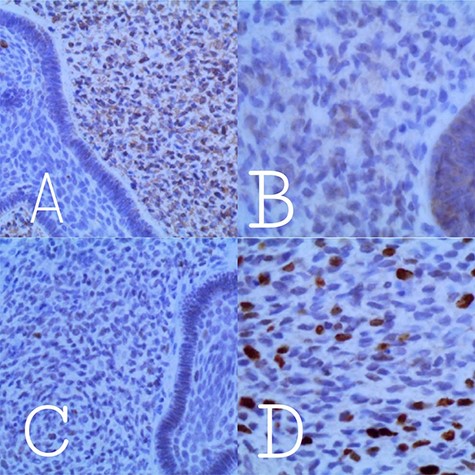
Reactivity to immuno-histochemical stains shows: A: positive reactivity to Vimentin in the mesenchymal component. B: negative reactivity to P53. C: negative reactivity to Bcl2. D: Reactivity to Ki67 in the mesenchymal component with a labeling index of 10–15%.
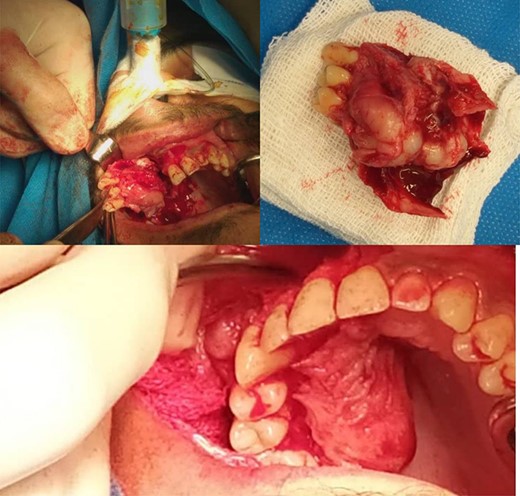
The excised specimen showing an irregularly shaped yellowish gray mass.
CASE PRESENTATION
A 21-year-old male patient presented with swelling in the right maxilla (Fig. 1). The patient had noticed this swelling for the first time 5 months ago in the palatine process of maxilla. This swelling has grown larger within these several months and has spread from the vestibule of the mouth reaching the upper right premolars. Orthopantomography revealed a radiolucent area with calcified lesions and resorption in the roots of the mentioned premolars, reaching the root of the canine as shown in (Fig. 2). Neck ultrasound revealed normal findings. Under topical anesthesia, an oval incision was performed. Histo-pathological findings are shown in (Fig. 3). Immunohistochemistry was performed using vimentin, B-cell lymphoma (Bcl-2), p53 and Ki-67.Vimentin was positive, whereas Bcl-2 and p53 were negative; Ki-67 was expressed by 10–15% of the mesenchymal cells (Fig. 4). In view of these histo-pathological and immunohistochemistry findings, a low grade AFS was diagnosed. After that, the patient underwent a right hemi-maxillectomy with clear margins (1.5–2 cm). Vestibular and palatal mucosal flaps were eradicated. The maxillary bone split from the lateral side of the 21st tooth toward the maxillary tuberosity with complete removal of the maxillary sinus up to the orbital floor. Then, antimicrobial gauzes were applied and we left the wound healing by secondary intention (Fig. 5). A second histo-pathological study confirmed the low grade AFS. The anterior and posterior surgical bone margins were focally involved by the tumor; therefore, another surgery was performed to fully remove the tumor. Because of the deep invasion of the tumor, the surgical procedure was followed by radiotherapy. A radiographic follow-up with head and neck computerized tomography after 3 months revealed that there were no metastases to the surrounding lymph nodes. Delayed reconstruction and rehabilitation should be taken into considerations.
DISCUSSION
AFS is a rare malignant odonto-genic tumor. It represents <5% of all odonto-genic tumors [1]. It was first described by Heath in 1887 [4]. To the best of our knowledge, about 100 documented cases of AFS have been reported. The majority of AF cases are seen in young patients, whereas AFS is seen in older patients [4]. The average age of AFS is about 26 years [4]. Clinically, AFS causes intra-oral and/or extra-oral swelling, which was the main symptom in our case [1]. Patients usually complain of a painful facial mass [2]. However, our patient’s mass was painless. Related symptoms may take from few months up to a year to appear obviously causing, sometimes, a facial deformity [4]. In our case, the tumor took about 5 months to reach a big mass. The majority of reported AFS cases have been located in the molar and premolar regions of the mandible [7], whereas in this report, the tumor was found within the maxilla which is considered a rare location.
Due to limited data on this tumor, an accurate treatment guideline is not recommended [7]. Surgical excision with clear and complete margins and long-term follow-up may be the standard management [4]. There is no strong evidence for the impact of adjuvant therapies in primary treatment of AFS [5]. Nevertheless, the patient received an adjuvant radiotherapy, as it may reduce recurrence rate and local invasion of the tumor [7].
Determination of fibrosarcoma malignancy depends on its degree of differentiation (histo-pathologic grading) [6]. And in view of our previously mentioned histo-pathological findings, our tumor’s degree was estimated as low grade. AFS has low potential for distant metastasis (only two reported cases), but a high reported recurrence rate of 37% and a mortality rate of 19% [2, 4]. Histologically, AFS is characterized by benign epithelial islands which are made up of columnar or cuboidal peripheral cells arranged in a palisading form with a malignant mesenchymal component, composed of ovoid and fusiform cells, in addition to plump and spindle stromal cells that show hyper-cellularity and nuclear polymorphisms associated with cytologic atypia, mitotic figures and anaplasia [1, 2]. Despite AFS has the last mentioned malignant mesenchymal component and a high labeling indices unlike AF, we still consider AF the main differential diagnosis of AFS as both have a biphasic nature and similarize in the benign epithelial tissue [2, 4]. The diagnosis of tumor malignancy was based on the morphological features and Ki-67 index for cell proliferation (10–15% in our case). AFS immuno-histochemistry usually shows positivity for p53 and Bcl-2 unlike the negativity in AF [4, 8, 9], but in our case, the negativity of immuno-staining for p53 and Bcl-2 can be attributed to the low grade nature of the tumor. Later reconstruction may require local or free flaps, cutaneous or mucosal, bone grafts, etc, according to the squeal of excision. Once reconstruction is performed, an implant-based rehabilitation may be performed [1].
CONCLUSION
Because of limited data and rarity of this tumor, an accurate management is still difficult to define. Although surgical resection is still the mainstream, adjuvant therapies should be into consideration to reduce recurrence and improve survival.
CONFLICT OF INTEREST
None declared.
Funding
None.
References
Author notes
The Guarantor: Amjad Soltany



