-
PDF
- Split View
-
Views
-
Cite
Cite
David Tovmassian, Linda Tang, Ahmer M Hameed, Jinna Yao, Peter Daechul Yoon, Taina Lee, Jerome M Laurence, Lawrence P K Yuen, Richard D M Allen, Howard Lau, Henry C C Pleass, Beware the band adhesion: an unexpected cause of double obstruction following intraperitoneal kidney transplantation, Journal of Surgical Case Reports, Volume 2020, Issue 8, August 2020, rjaa239, https://doi.org/10.1093/jscr/rjaa239
Close - Share Icon Share
Abstract
Small bowel obstruction (SBO) following intraperitoneal renal transplantation, either solitary or due to simultaneous pancreas-kidney transplantation, is a known complication. While SBO is most commonly due to adhesions, there have been documented cases of internal herniation following simultaneous pancreas-kidney transplantation with enteric drainage due to the formation of a mesenteric defect. We present a unique complication in which the transplant ureter has caused strangulation and necrosis of a length of small intestine. The transplant ureter was mistaken for a band adhesion and divided. Post-operative anuria signalled this difficult diagnosis. Subsequent re-look laparotomy and ureteric reimplantation with Boari flap were required. Therefore, it is important to consider the ureter as a cause of internal herniation in kidney transplant patients and recognize that a band adhesion within the pelvis may in fact be the transplant ureter, obstructing a loop of small intestine beneath its course.
INTRODUCTION
Small bowel obstruction (SBO) complicated by strangulation and necrosis is a surgical emergency with significant morbidity and mortality [1].The most common cause of SBO is adhesions; however, other causes need to be considered especially in the transplant population [2]. SBO following SPK due to internal herniation is a rare but documented complication when undergone with enteric drainage of the pancreas due to the formation of a mesenteric defect [3]. There is a single case report previously published of internal herniation with an obstructed small bowel loop, beneath a transplant ureter [4]. To our knowledge, this is the first reported case where the ureter has been mistaken for a band adhesion and divided.
Accidental transection of the transplant ureter is a serious complication which can be difficult to diagnose and treat. Technique of ureteric reimplantation is dependent upon the location of transection, size of bladder and blood supply of the ureter [5].
We report a case of SBO with necrosis secondary to internal herniation beneath the ureter of the transplant kidney leading to the obstruction of the renal allograft (double obstruction). This was complicated by accidental transection of the transplant ureter which was mistakenly identified as a band adhesion.
CASE REPORT
A 57-year-old female who underwent SPK (1998) and developed eventual loss of function of both renal and pancreas grafts secondary to chronic rejection. She underwent a live donor renal transplantation (2015) placed in the left iliac fossa via midline laparotomy and transperitoneal approach. Her failed pancreatic graft remained in situ, on the right side. Renal function remained normal until 1 week prior to her acute presentation.
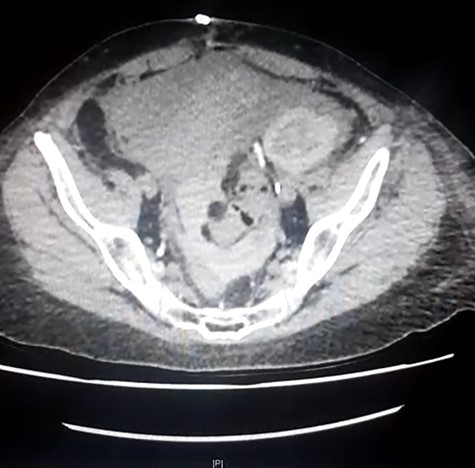
She presented to her local hospital due to sudden onset of severe abdominal pain with associated nausea, vomiting and diarrhoea. She was tachycardic though normotensive on presentation and found to have generalized severe abdominal pain. CT imaging revealed an SBO with an evidence of ischaemia as well as an obstructed ureter and renal collecting system within the allograft (Fig. 1). She underwent laparotomy, division of band adhesion in the left pelvis and 1.2 m of small bowel resected due to ischaemic necrosis with an end-to-end hand sewn anastomosis.

Initial CT demonstrating SBO and obstructed renal allograft/ureter (double obstruction).
Post-operatively, she was noted to be anuric and the quaternary referral centre with transplantation services was contacted for transfer.
After transfer, the patient was noted to have ongoing severe abdominal pain in the lower abdomen and ongoing anuria. She was haemodynamically stable, afebrile and presentation was consistent with acute graft injury secondary to ischaemic bowel.
On arrival, her haemoglobin was 120 g/L with white cell count 14.7 × 109/L, and CRP 157 mg/L, creatinine 348 umol/L (baseline 80), eGFR 10 mL/min, Urea 10.1 mmol/L and potassium 5.2 mmol/L.
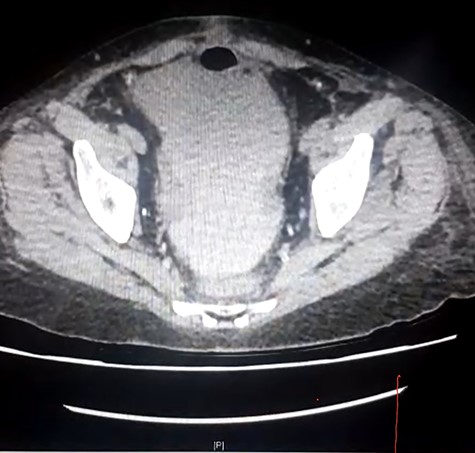
Repeat CT imaging with IV contrast at the referring hospital prior to transfer revealed large volume free fluid intraperitoneally with ongoing dilatation of the renal collecting system which was contrast filled. The distal ureter was not seen entering the bladder. The free fluid in the pelvis also demonstrated increased density raising concern for haematoma or possibly intravenous contrast (Figs 2 and 3).
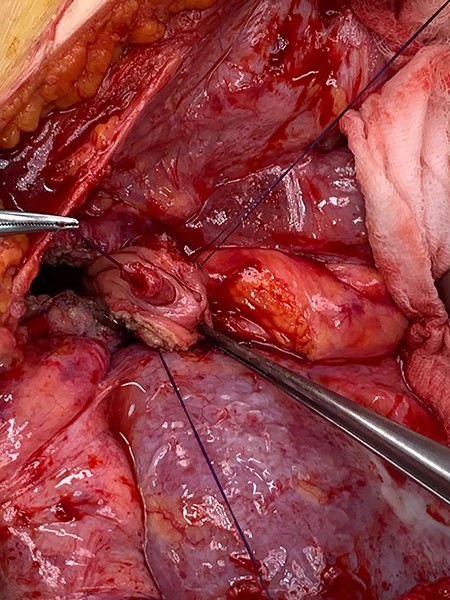
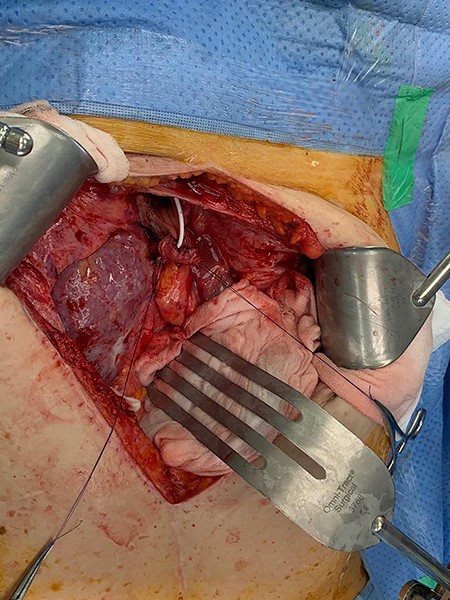
The patient underwent a repeat laparotomy 48 hours after initial operation. Findings during the case included large volume of intraperitoneal urine with a complete transection of the transplant ureter (Fig. 4). The transplant ureter had been mistaken for a band adhesion, and the small bowel had clearly herniated beneath ureter, causing obstruction to the kidney and infarction of the strangulated small bowel. The ureter was reimplanted onto the bladder with the formation of a Boari flap, stented, without tension, having first excised the end of the diathermied ureter to ensure viable and well-vascularized tissue (Figs 5–8).
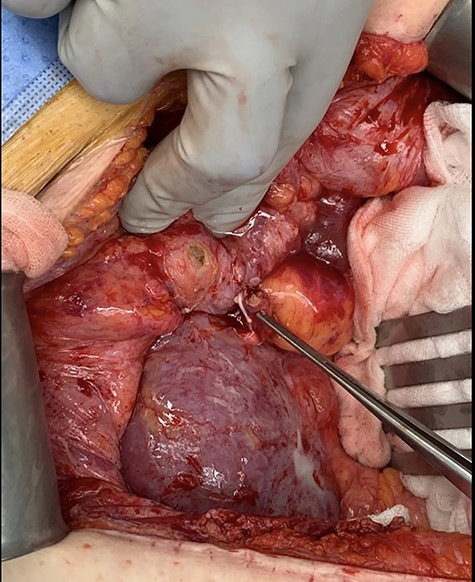
Intraoperative photo demonstrating divided transplant ureter with diathermy burn seen on bladder at previous site of anastomosis.
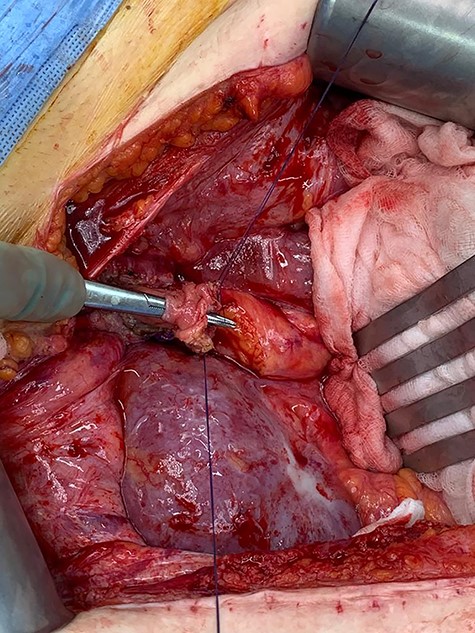
Forceps through bladder demonstrating route of ureter through Boari flap.
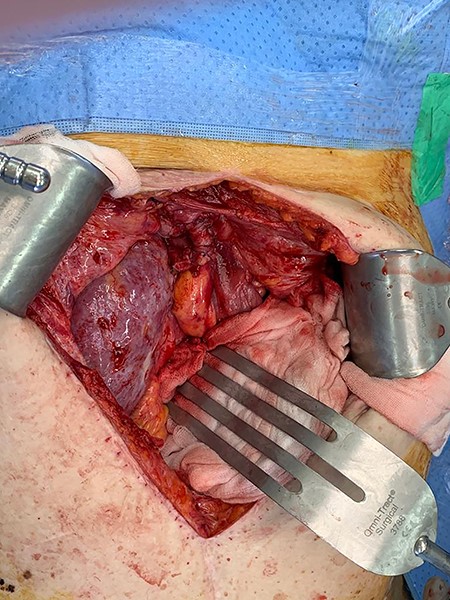
The patient recovered well post-operatively with immediate function of the renal graft and rapid normalization of the creatinine within 24 hours. She was discharged home post-operative Day 5 with an IDC in situ and returned for a CT cystogram and removal of stent. Unfortunately, her recovery was further complicated by stricture of the reimplanted transplant ureter. The ureteric obstruction was decompressed with a nephrostomy tube. A nephrostogram, antegrade stent insertion and removal of nephrostomy were subsequently performed. Her renal function normalized and her IDC removed. She was discharged home with urological follow-up.
DISCUSSION
Following SPK transplantation, there is significant morbidity with 26% of recipients requiring repeat laparotomy within 3 months [6]. Late complications include vascular, infection, pancreatitis, anastomotic leaks and bowel obstruction [7]. A case report published by Anderson et al. outlines a case of internal herniation following intraperitoneal renal transplantation [4]. There is a report of accidental division of the transplant ureter during laparoscopic surgery for lymphocoele drainage; however, there is no reported case of accidental division of transplant ureter believing it to be a band adhesion [8].
The diagnosis of SBO can be readily made with clinical criteria and imaging such as CT [9]. As these immunosuppressed patients mask both symptoms and signs, transfer or discussion with a transplanting unit is recommended. It is important for clinicians when evaluating transplant recipients with SBO, especially those with intraperitoneal grafts to have a high index of suspicion for internal herniation as it has been reported to have a strangulation rate over 40% [4]. Prompt treatment is necessary once diagnosis has been established. Laparotomy division and/or reduction of the small intestine to allow for adequate exposure to identify structures is a safe initial course of action.
Repair of a divided transplant ureter is a unique and complex procedure with multiple considerations for reimplantation [5]. In our case, a Boari flap was utilized due to the need for extended length; however, the ureteric repair should be tailored to the individual. Urological surgery input may be required.
Transplant recipients pose a unique population in which diagnosis of complications is a challenge due to the presence of immunosuppression. Not all clinicians have adequate exposure to transplant recipients and therefore may be unaware of potential complications and anatomical considerations in these patients. It is therefore important to have a high index of suspicion when evaluating possible complications in transplant recipients and consider transfer to transplant referral centres where appropriate.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



