-
PDF
- Split View
-
Views
-
Cite
Cite
Joshua Wong, Nicholas Farkas, Sherif Monib, Simon Thomson, A challenging case of a chyle leak following axillary lymph node clearance, Journal of Surgical Case Reports, Volume 2020, Issue 8, August 2020, rjaa286, https://doi.org/10.1093/jscr/rjaa286
Close - Share Icon Share
Abstract
Chyle leak following axillary lymph node clearance is a rarely reported complication. We present a case of chylous leakage following axillary lymph node clearance, which was diagnosed on clinical grounds. Surgical re-exploration was undertaken due to ongoing high output. However, the chylous leak recurred post-operatively, if at a lower rate. The patient was subsequently managed successfully with conservative measures, primarily utilizing regular aspiration and compression bandaging to the axilla.
INTRODUCTION
Chyle is a turbid, milky substance carried in the lymphatic system direct from the intestine. It has a high content of protein, fat and white blood cells. Chylous leaks occur more commonly secondary to head, neck or intra-thoracic surgery. However, such leaks also very rarely occur following axillary or breast surgery. Chylous leaks are thought to stem from iatrogenic injuries at the time of surgery due to aberrant anatomy of the thoracic duct and its tributaries. Management options vary with both conservative and surgical options available to clinicians.
CASE REPORT
A 71-year-old female presented with 70-mm left breast invasive ductal carcinoma. Her medical history included early dementia, hypothyroidism and rheumatoid arthritis, with World Health Organization performance status 2. She initially underwent a left mastectomy and sentinel node biopsy. There were no intra-operative complications and post-operatively she recovered well.
Histopathology confirmed 77 mm, grade III invasive ductal carcinoma with one involved sentinel lymph node biopsy (SLN). Subsequent staging computed tomography scan was clear. The patient proceeded to uneventful axillary clearance to level III, 7 weeks later, a Redivac suction drain was left in the axilla. All of the remaining 18 lymph nodes excised showed no evidence of malignancy on subsequent histology.


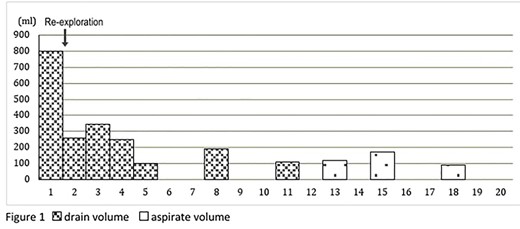
Graph demonstrating the drainage and aspiration volumes for this patient following axillary clearance.
Post-operative day (POD) 1 on examination 800 ml of a milky fluid was present in the drain, indicative of a chyle leak. Other imaging modalities such as lymphoscintigraphy and biochemical studies were not considered as it was felt that these would not alter management. In view of the high output, the decision was made for a re-exploration of the axilla on POD 2. Intra-operatively, the source of the leak was localized to posterior to the axillary vein next to the chest wall, although the specific vessel could not be identified within the residual tissue edge. Ligaclips and suture ligation of the area appeared to control the leak intra-operatively. The Redivac was changed to a Blake low-pressure suction drain and a pressure bandage was applied.
Post-operatively, however, the chylous leakage continued but at a reduced rate. The drain remained in situ initially and the patient progressed well post-operatively, albeit with some oozing from around the Blake drain site, which was managed by removal of the suction and stoma bag placement, prior to discharge on POD 5 with nursing input in the community (Figs 1–3).
From POD 10, the patient developed an axillary chyloma despite flushing the drain and continued leakage into the stoma bag. On POD 11 the drain was removed and the pressure dressing re-applied. After 2 days, 120 ml of chylous fluid aspirated from the axilla, and a further 170 ml of chylous fluid was aspirated from the axilla on POD 15. On POD 18, a further 90 ml of chylous fluid aspirated and the collection was noted to be more loculated than before.
The patient re-attended the breast clinic on POD 20 and no further evidence of chyle leak was noted. She was subsequently referred to the clinical oncology team for consideration of chemotherapy and radiotherapy.
DISCUSSION
Iatrogenic injury during axillary surgery resulting in a chylous leak is extremely rare with quoted incidents of <0.5% [1]. Our case highlights several important points regarding diagnosis and management.
Because of the high initial output of milky fluid, the diagnosis of chyle leak was clear and whilst in the majority of reported cases biochemical analysis of the fluid was conducted [2], it was felt no alteration to management would have occurred in our case. Likewise, lymphoscintigraphy was considered, but again felt that this modality would not alter management. We suggest that such modalities should be utilized if there is any clinical uncertainty as to the nature of the fluid. With active leakage, the site should be identifiable at further exploration, but lymphoscintigraphy could help anatomically if, for example, there had been a significant delay before re-exploration and extensive tissue induration anticipated.
Some authors report the successful use of suction [3, 4]. However, it is questionable whether a suction drain may exacerbate symptoms, with the vacuum acting as a catalyst for ongoing output. We opted for changing to a low-pressure suction system with direct pressure, but noted a reduction in chylous output once the suction drain had been removed. The collection was able to loculate, offering an element of tamponade.
A major challenge in this case related to the patient’s dementia as opposed to the leak itself. There were instances of her forgetting to protect the drain and whilst change to a stoma bag aided with this, with such high outputs leakage of this became a problem. Regular clinic reviews and subsequent aspirations ensured that chylous collections were controlled and enabled accurate volumes to be recorded. A further patient-specific factor related to the implementation of a low-fat diet, which is recommended to help reduce lymphatic flow. With the patient already very thin and with ongoing poor oral intake, ensuring such a diet was in place was not practical. This meant relying on other strategies to manage the leak.
As with number of other cases, the high chylous output prompted a return to theatre for re-exploration [5–7]. Although drain output decreased post-surgery, this did not immediately resolve the leak and continued conservative management with a reduction in suction pressure and pressure dressings ultimately was successful.
CONCLUSION
Chyle leak is a clinical diagnosis, which can be managed conservatively. Re-exploration may be considered for high output > 500 ml/24 h, although it may not highlight the point of leakage.
We advocate the use of compression packing and bandaging to the axilla in addition to low-pressure suction or free drainage or aspiration. Low-fat diet may also be useful, but taking in consideration patient-specific factors is imperative when managing each individual case.
AUTHOR’S CONTRIBUTIONS
All authors were involved in patient’s management, literature review as well as manuscript editing.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
NOTES
This article has not been presented at any symposium or conference to date.



