-
PDF
- Split View
-
Views
-
Cite
Cite
Gregory Wu, Azeem Yousaf, Evan Kessler, Eric Seitelman, Rajiv Datta, Recurrent lymphoepithelial cysts after parotidectomy in an undiagnosed HIV-positive patient, Journal of Surgical Case Reports, Volume 2020, Issue 8, August 2020, rjaa300, https://doi.org/10.1093/jscr/rjaa300
Close - Share Icon Share
Abstract
A benign lymphoepithelial cyst (BLEC) is defined as a rare, benign lesion composed of single or multiple cysts found within salivary glands or the lateral cervical area. Increasing reports suggest an association between BLEC and human immunodeficiency virus (HIV), although its pathogenesis remains unclear. We report a 51-year-old male who presented with recurrent bilateral BLECs after initial parotidectomy of cyst. An HIV panel was then performed with a positive result. We review the surgical and medical managements of BLEC while also discussing further treatment recommendations. Clinicians should be aware that BLEC recurrence postparotidectomy may be the initial presenting symptom of HIV in a patient with no risk factors.
INTRODUCTION
A benign lymphoepithelial cyst (BLEC) is a rare and slow-growing lesion composed of single or multiple cysts within lymph nodes associated with salivary glands [1]. These cysts present as unilateral painless swelling and are found in the lateral cervical neck and salivary glands. The diagnosis of BLEC often requires evaluation of the history, physical exam and fine need aspiration biopsy for histopathological analysis [2]. While the incidence of a BLEC is low, there has been increasing evidence in the literature that suggests an association of BLEC with human immunodeficiency virus (HIV). We report a case of a 51-year-old male with no significant reported risk factors who was found to be HIV positive after the unusual presentation of bilateral BLEC recurrences postparotidectomy.
CASE REPORT
A 51-year-old male smoker with no significant medical history or risk factors for immunocompromised state presented with concern for a 12-month progressing right cheek swelling unresponsive to antibiotics. The patient denied dyspnea, dysarthria, dysphagia, dysphonia and xerostomia. Family history was non-contributory and the patient was married for 12+ years with children.
Computed tomography (CT) with contrast (Fig. 1) showed a right parotid gland fluid collection identified within the superficial lobe of the parotid gland with enlarged lymph nodes present in various levels of the neck. Fine-needle aspiration (FNA) revealed a cyst of the right parotid gland. A right superficial parotidectomy with nerve monitoring was performed and a well-circumscribed mass was excised. Pathology revealed a BLEC of the right superficial parotid measuring 3.5 × 2.5 × 2.1 cm.
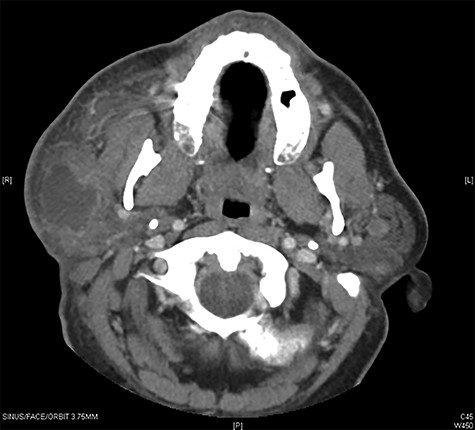
Maxillofacial Axial CT with contrast in the area of clinical interest demonstrating a 4 × 4.4 × 2 cm (AP, vertical transverse) well-circumscribed lesion in the right parotid superficial gland.
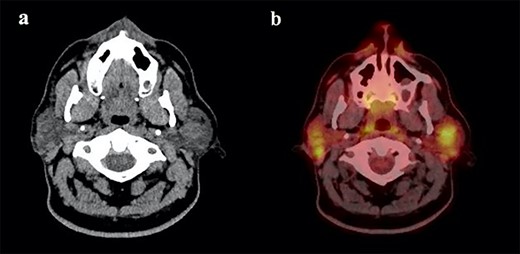
(a) Maxillofacial Axial CT with contrast showing multiple bilateral parotid gland lesions demonstrating internal enhancing septations with the largest lesion located in right parotid tail, measuring 1.9 x 2.1 cm and (b) associated PET CT scan showing bilateral hypermetabolic parotid lesions measuring up to a maximum standardized uptake value (SUV) of 10.0 on the left and 9.0 on the right.
The patient presented 6 months later with progressive bilateral cheek swelling, more significant on the right side. Repeat CT revealed multiple bilateral parotid gland lesions with the largest located within the right parotid tail (Fig. 2a). Positron emission tomography (PET) scan was ordered to rule out other diagnostic considerations including primary parotid tumors such as Warthin’s tumor or non-Hodgkin lymphoma, or secondary malignancy. Bilateral hypermetabolic parotid lesions were identified along with diffuse bilateral cervical adenopathy (Fig. 2b). Findings suggested bilateral BLEC which raised suspicion for a potential immunosuppressive state. An HIV panel was performed with a positive result. The patient underwent initial local aspiration and drainage to palliate his symptoms of cheek discomfort and treatment for HIV was discussed. Patient has since been placed on HIV medication for management and his bilateral cysts and lymph nodes have reduced in size at follow-up visits with no signs of further recurrence.
DISCUSSION
Lymphoepithelial cysts are benign lesions first described by Hildebrandt in 1895. To date, around 100 cases have been reported [1]. In a large majority of these, patients presented with unilateral swelling and requested evaluation for cosmetic purposes. While these lesions often have a benign presentation, they may undergo lymphomatous transformation and thus require frequent monitoring [3].
Diagnosis of BLEC is often challenging, and most are only classified after surgical excision and histopathology evaluation of the mass. Other salivary gland diseases can often be considered in the differential of BLEC and are shown to be associated with immunocompromised diseases. Some of these pathologies include parotitis, intraparotid lymphadenopathy, salivary gland neoplasms and sicca syndrome. Increasing reports in literature state that BLEC is among this list of HIV-associated pathologies and advocate its presentation as a guiding diagnostic indicator of HIV.
Management of BLEC is debated and requires the differentiation between an isolated BLEC and HIV-associated BLEC. Patients at concern for HIV or who present with HIV have options, such as repeated aspiration and drainage, radiation therapy, sclerotherapy, highly active antiretroviral therapy (HAART) pharmacotherapy and surgery. Repeated FNA of the cysts can be performed but has shown a 100% recurrence rate within weeks or months [4]. Sclerotherapy is an option where the cysts are injected with sclerotic agents, such as sodium morrhuate, doxycycline, ethanol, bleomycin and picibanil [5]. Antiretroviral therapy (HAART) has shown to be an effective option in treating the underlying cause of HIV-associated BLEC, with studies showing a dramatic reduction in the size or elimination of parotid cysts after its initiation [6].
Despite the above options, surgery is still considered the most definitive treatment and gold standard. Enucleation is described as a procedure where the cyst is dissected off the surrounding parotid gland, but recurrence has been reported [7]. A better option for cyst removal is a superficial parotidectomy where the superficial lobe of the parotid is excised with careful preservation of the facial nerve. Shaha et al. performed a retrospective review of 35 parotidectomies and found a 100% complete response rate with no recurrence at 6 year follow-up [8].
Though it is documented in the literature that BLEC may be the initial presentation of HIV, our patient had reported zero risk factors that would put him at risk for immunosuppressed state. In a patient who presents with cheek swelling and a unilateral and singular cystic lesion suggestive of BLEC, we suggest that HIV panel should be performed regardless of any reported risk factor or number of cysts at presentation.
This case is important because of the unusual presentation of recurrent cysts in both parotid glands after parotidectomy of a single, unilateral lesion. Extensive review of the literature and databases reveal no other reports of cyst recurrence after the initial superficial parotidectomy of the cyst. We propose that parotidectomy may be optimal in immunocompetent patients, but may be insufficient for immunocompromised patients. Because our patient represented with multiple bilateral cysts, we believed repeat excision or drainage would have led to further recurrence. Therefore, we decided to manage his bilateral cysts with HIV medication which has led to a reduction in the size of cysts, with no evidence of recurrence at follow-up visits.
CONCLUSION
Clinicians should be aware that the reappearance of BLEC after initial surgical excision of a singular cyst may be the initial presentation of HIV even in a patient with no reported risks. The combination of parotidectomy and systemic management should be further considered as the standard in the management of symptomatic BLEC in patients with HIV in order to prevent recurrence or malignant transformation.
Conflict of interest statement
None declared.
Funding
None.



