-
PDF
- Split View
-
Views
-
Cite
Cite
Alessandro Russo, Vito Coco, Stefano Zaffagnini, The effect of autologous adipose derived mesenchymal stem cell therapy on juvenile osteochondritis dissecans of the patella: a case study, Journal of Surgical Case Reports, Volume 2020, Issue 8, August 2020, rjaa274, https://doi.org/10.1093/jscr/rjaa274
Close - Share Icon Share
Abstract
A prospective analysis of the effect of autologous adipose derived mesenchymal stem cell (AD-MSCs) therapy in the treatment of a juvenile osteochondritis dissecans (JOCD) of the patella. After failed conventional management of JOCD, a 13-year-old patient undergoes intra-articular MSC therapy. Repeated magnetic resonance imaging analyses showed regeneration of cartilage. In this report, the use of AD-MSCs, after unsuccessful conventional JOCD management, resulted in structural, functional and pain improvement. These results highlight the possibility to avoid surgery treatment in JOCD patella treatment.
Introduction
Juvenile osteochondritis dissecans (JOCD) is a disorder of the subchondral bone and overlying articular cartilage, that most commonly affects the knee of active skeletally immature patients (defined by open physis). In particular it occurs when a small piece of subchondral bone below the articular cartilage begins to be different from its surrounding area due to a disturbance of the local blood supply and as a result, the overlying joint articular cartilage becomes susceptible to injury. Finally, a small fragment of bone and the cartilage covering it may begin to crack, resulting in delamination and sequestration with or without articular cartilage involvement and instability [1]. JOCD lesions are often stable, with an intact articular surface, and have the greatest potential to heal with conservative treatment. Most commonly, JOCD lesions are seen in the posterolateral aspect of the medial femoral condyles of the knee (50–80%), location in the patella is rare (~2%) and is predominantly in the lower portion; OCD lesions are often described as stable or unstable with stable lesions considered to be suitable for nonoperative conservative management. De Smet et al. [4], using a T2 weighted magnetic resonance imaging (MRI) technique, noted four criteria with an observed correlation with instability—(i) a high signal line surrounding the lesion, (ii) a focal area of overlying articular cartilage defect, (iii) a fracture of the articular cartilage and (iv) presence of subchondral cyst of 5 mm or greater in diameter. The aim of this study is focus on a possible new treatment for JOCD of patella.
Case Report
A 14-year-old female dancer presented with increasing right knee pain and functional disability without any trauma. Her pain was retropatellar pain that often radiated medially or laterally from the patella, exacerbated by climbing stairs, running and squatting. She was unable to perform any sports activities. Examination revealed peripatellar tenderness and crepitus, full range of motion and the knee was stable. Radiological examination included both MRI and computed tomography of the knee were performed at the beginning. MRI showed osteochondritis dissecans at the area at the superolateral facet of the patella in the deep subchondral area as shown in Fig. 1. This was appropriately treated conservatively with 6 months of reduced load and protected weight bearing without relief of symptoms. She quit sport activity for 2 years and then another MRI was performed Fig. 2. After 2 years we opted for adipose-derived mesenchymal stromal cells (AD-MSCs) intra-articular therapy according to the procedure described by Tremolada et al. [9]. The patient’s parents were given written information regarding the use of AD-MSCs therapy, including relative risks of this therapy and also relevant treatment alternatives that could otherwise be explored. Postoperative radiological evaluation was performed at 6 months and 12 months after AD-MSCs procedure as shown in Figs. 3 and 4. Postoperative clinical evaluation was performed using IDKC, Lysholm and Tegner scores (Table 1). After surgery, patients began a McConnell program of lateral retinacular stretching, patellar taping and vastus medialis obliquus muscle exercises. The patient was encouraged to swim and cycle to reduce impact loading. Using AD-MSC, she reported a complete relief of pain after 1 year from the procedure. Routine MRI follow-up 2 years later showed evidence of appreciable improvement in cartilage volume and osteochondral architecture at the site of injury. Early MRI T2 mapping at 6 months indicated that the area of cartilage regeneration exhibited high water content suggestive of immature cartilage or fibrocartilage morphology. Later T2 mapping at 18 months after the procedure, indicated progressive maturation of cartilage from deep to superficial layers with more hyaline like cartilage morphology. Limitations of the study are lack of arthroscopic intra-articular visualization and classification of the patella lesion.
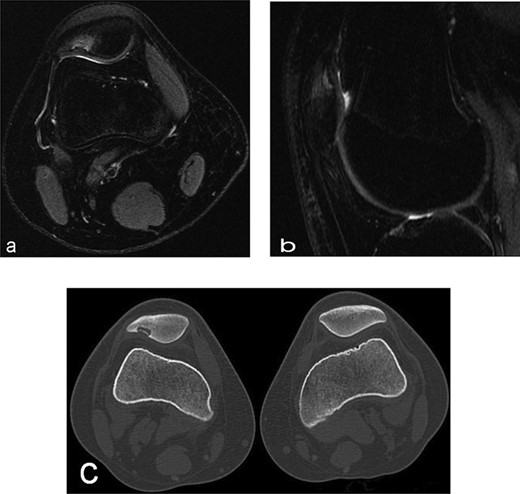
Radiographs of the patient’s knee at 14 years old (a) Axial T2-weighted MRI sequences (b) sagital T2-weighted MRI sequences showed abnormality area at the superolateral facet of the patella in the deep subchondral area, this area of altered signal, hypointense in T1 and hyperintense in T2 with a shaded surrounding edema, was oval in morphology and had a craniocaudal extension of about 12 mm and transversal about 10 mm, the lesion interrupted the corresponding patellar articular cartilage which appears swollen in this position (c) axial computed tomography scan showed loss bone at that same point of patella in the right knee.
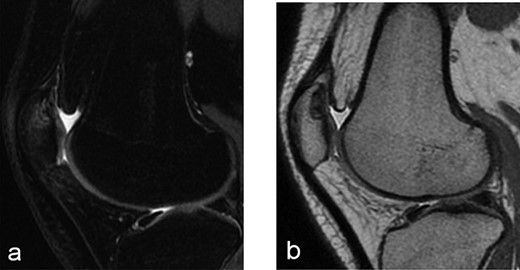
Radiographs after 2 years at 16 years old (a) sagital T2-weighted MRI sequences (b) sagital T1-weighted MRI sequences showed the area was still the same at the superolateral facet of the patella in the deep subchondral area.
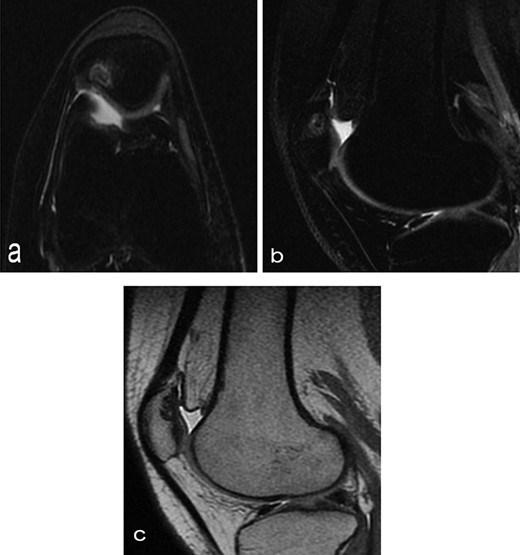
Six months after MSC treatment in (a) axial and (b) sagital T2-weighted of MRI T2 sequences the OCD in patella showed that area of cartilage in regeneration and fill of high water content suggestive of immature cartilage or fibrocartilage morphology (c) same lesion in sagital T1 weighted MRI sequences.
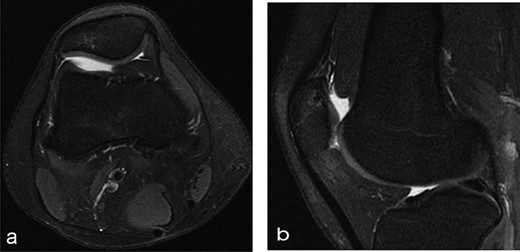
Twelve months after MSC treatment in (a) axial and (b) sagital T2-weighted of MRI T2 sequences the OCD in patella showed that area was almost regenerated with good fibrocartilage morphology.
IKDC, Lysholm and Tegner scores reported preoperative, 6 months postoperative, 12 months postoperative
| Scores . | Pre-op . | 6 months post-op . | 12 months post-op . |
|---|---|---|---|
| IKDC | 23 | 80.5 | 98.9 |
| LYSHOLM | 28 | 99 | 100 |
| TEGNER | 0 | 8 | 8 |
| Scores . | Pre-op . | 6 months post-op . | 12 months post-op . |
|---|---|---|---|
| IKDC | 23 | 80.5 | 98.9 |
| LYSHOLM | 28 | 99 | 100 |
| TEGNER | 0 | 8 | 8 |
IKDC, Lysholm and Tegner scores reported preoperative, 6 months postoperative, 12 months postoperative
| Scores . | Pre-op . | 6 months post-op . | 12 months post-op . |
|---|---|---|---|
| IKDC | 23 | 80.5 | 98.9 |
| LYSHOLM | 28 | 99 | 100 |
| TEGNER | 0 | 8 | 8 |
| Scores . | Pre-op . | 6 months post-op . | 12 months post-op . |
|---|---|---|---|
| IKDC | 23 | 80.5 | 98.9 |
| LYSHOLM | 28 | 99 | 100 |
| TEGNER | 0 | 8 | 8 |
Discussion
There are many studies about JOCD treatment but rare isolated and limited cases series are reported in the literature concerning the management of OCD of patella in young patients, using the conventional techniques with short-term follow-up [6]. A similar approach and good results have been reported by Freitag et al. [5] but in their case the patient had a lesion of medial femoral condyle and matrix autologous chondrocyte implantation failed as first option treatment. The characteristics commonly associated with failure of nonoperative treatment including skeletal maturity, large lesion size (>160–200 mm2), abnormal location and primary mechanical symptomatology [3]. Treatment of patella articular cartilage lesions is challenging owing to the complexity of the patellofemoral joint, the limited capacity to heal and its complex surgical approach of the area. The failure rates of conservative treatment have been reported as over 50% [8]. Surgical management of stable lesions that fail conservative management can include drilling, perforation, curettage and fixation using compression screws or bioabsorbable implant/nails with poor efficacy. The difficultly location and matching the shape of an articular surface as patella joint, leads many surgeons to prefer surface allograft transplantation or cell-based therapies such as cell-based therapy broadly encompasses second generation autologous chondrocyte implantation (ACI) or particulated juvenile allograft cartilage over allograft transplantation or autograft transfer [2]. These procedures are not free of complication, for example, ACI has some disadvantages: requirement of regional or general anesthesia (for harvesting and implantation), difficulty and slow time in obtaining adequate number of chondrocyte and morbidity of the donor site [7]. All this new advanced treatment were based on an invasive intra-articular surgery although the use of AD-MSCs therapy could be a solution in particular as second option after conservative treatment failed and before to use other more invasive.
Conclusion
There are not guidelines on treatment of JOCD of the patella. No study on the treatment of it using AD-MSCs has been published to date. The disease modification and structural improvement in the underlying articular pathology observed in this case study, suggests that AD-MSCs therapy could be a valid option using a simple injectable technique without risks and complications due to invasive intra-articular surgery among the new and old generations therapies.
Conflict of interest statement
None declared.
FUNDING
None.



