-
PDF
- Split View
-
Views
-
Cite
Cite
Raouf Fayisall Geraldo, Boyodi Katanga Tchangai, Efoé-Ga Yawod Olivier Amouzou, Fousseni Alassani, Birega Koutora, Abossisso Sakiye, Kokou Kouliwa Kanassoua, David Ekoué Dosseh, Miliary abscess of the liver: unusual complication of intestinal perforation, Journal of Surgical Case Reports, Volume 2020, Issue 8, August 2020, rjaa278, https://doi.org/10.1093/jscr/rjaa278
Close - Share Icon Share
ABSTRACT
Miliary abscess of the liver represents a rare presentation of multiple liver abscesses. They often occur in immunosuppressed patients, or those with underlying liver disease. We report the case of a 22-year-old patient, without known immunodeficiency factors, surgical history or notion of tuberculous contacts, who was admitted for generalized peritonitis and ileal perforation. An ileostomy was performed. The infectious syndrome persisted in post-operative period, associated with painful hepatomegaly. An contrast-enhanced abdominal CT scan led to the diagnosis of miliary abscess of the liver. A blood culture isolated Escherichia coli. The treatment included antibiotics and the clinical evolution was favorable. The follow-up abdominal CT scan was normal. Intestinal continuity was restored without complications. Miliary abscess of the liver is rare and requires rapid diagnosis. The treatment is based on antibiotic therapy.
INTRODUCTION
Miliary abscess of the liver is defined by the presence of diffuse micro-abscesses within the liver parenchyma (usually 1–3 mm in diameter). The clinical signs are non-specific. CT scan with contrast can provide the diagnosis. Prompt diagnosis and initiation of treatment improves the prognosis. The treatment is based on antibiotic therapy. This is a rare condition and usually caused by Yersinia enterocolitica [1, 2]. It occurs most often in immunosuppressed patients. Three main routes of contamination are described: arterial, venous and biliary.
We report here the case of miliary abscess of the liver due to Escherichia coli in an immunocompetent adolescent. The objectives of this report are to describe the mechanism of occurrence, the management and to review the literature.
CASE REPORT
A 22-year-old male patient was admitted for generalized abdominal pain associated to bilious vomiting and fever for 3 days duration. He had neither known immunodeficiency, nor history of exposure to tuberculosis. He was healthy and took no medications prior to this acute illness. The patient reported an abdominal trauma in the near the umbilicus during a football game the week before admission. The clinical examination at the entrance revealed a temperature of 39°C, a tachycardia at 106 pulsations per minute. General appearance was normal. There was abdominal pain with tenderness to palpation. He had no other associated signs or symptoms. On admission, a plain abdominal X-ray demonstrated pneumoperitoneum. The white blood cell count was 11.200/mm3. He was taken emergently to the operating theater for exploratory laparotomy. At the opening of the peritoneum, there was digestive fluid, and an oval ileal perforation of about 0.5 cm in diameter on the anti-mesenteric side about 5 cm from the ileocecal junction. An intestinal resection was performed with terminal ileostomy and drainage of the peritoneal cavity. Medical treatment was started made of intravenous analgesics and antibiotics (ciprofloxacine 200 mg every 12 h and metronidazole 500 mg every 12 h).
The post-operative status was marked by the persistence of SIRS, a deterioration of general appearance, pain in the right hypochondrium and hepatomegaly noticed on the eighth post-operative day. No jaundice was noted. A contrast-enhanced abdominal CT scan was performed showing small, homogeneous hypodensities disseminated in the liver parenchyma giving the appearance of miliary abscess. There was no lymphadenopathy or associated ascites (Fig. 1).
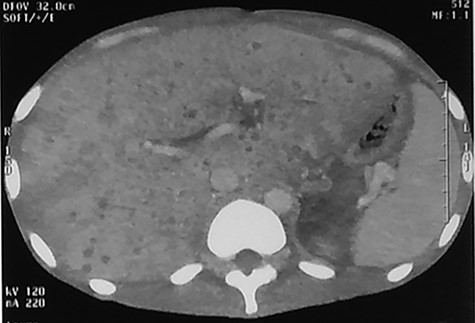
Abdominal CT injected at portal phase performed on 10th postoperative day showing millimetric, homogeneous hypodensities disseminated in the hepatic parenchyma.
CRP was positive at 350 mg/L. The blood count revealed leukocytosis at 15 620/mm3, predominantly neutrophils. Blood culture has isolated E. coli. The Koch bacillus test was negative, so was the retroviral serology. The diagnosis was miliary abscess of the liver. Treatment was begun with intravenous antibiotics: Imipenem (1 g every 8 h), amikacine (2 g in 250 mL of isotonic glucose serum) and metronidazole (500 mg every 8 h). The inflammatory syndrome decreased after 10 days of treatment. Oral therapy was started for a period of 2 weeks, using amoxicillin-acid clavulanic tablets (one tablet every 12 h) and metronidazole tablets 500 mg (one tablet every 8 h).
Abdominal CT scan at 3 months showed disappearance of the miliary abscess and also of the hepatomegaly (Fig. 2).
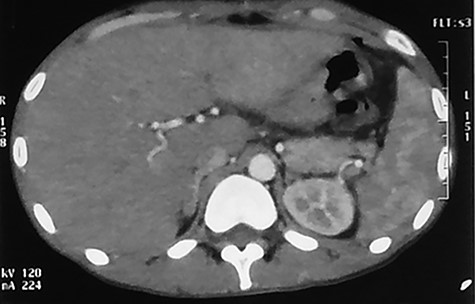
Abdominal CT scan (arterial phase) performed at 90th day after the beginning of the antibiotherapy showing normal liver parenchyma.
The intestinal continuity was restored 2 months later with simple operative follow-up. Histological examination of the intestinal biopsy was non-specific.
DISCUSSION
Miliary abscess of the liver is a rare type of multiple abscesses of the liver, and is characterized by abscesses number (more than eight), diameter (less than 2 mm) and particular dissemination in the hepatic parenchyma. Few cases are reported in the literature. It occurs mainly in young population [2] with male dominance [3]. Miliary liver abscess is often associated with immunosuppressive conditions including diabetes, hemochromatosis and alcoholism [1–3]. However, no such condition was discovered in this case.
The typical presentation which may suggest the diagnosis of miliary liver abscess includes abdominal pain and hepatomegaly [4]. Two variations in presentation have been identified, which depend on the type of bacteria causing the infection. Staphylococcus, Enterococcus and Yersinia enterocolitica are known to produce high fever (>39°C) and a severe inflammatory syndrome [1, 2, 5]. On the other hand, cases of miliary liver abscess caused by Mycobacterium tuberculosis follow a more indolent course with low-grade fever and little or no systemic inflammatory response syndrome [6]. The diagnosis is confirmed by contrast-enhanced CT scan showing 1–3 mm, homogeneous hypodensities disseminated in the hepatic parenchyma [4]. This must be distinguished from metastatic miliary malignancy, as described by Pichon et al. [8].
The treatment is based on antibiotics, with follow-up CT scan to confirm clearance of disease. The typical treatment includes penicillins (imipenem), imidazoles (metronidazole) and third generation quinolones (ciprofloxacin) for a duration of 2 months [9, 10]. The regression of the clinical symptoms is generally noticed after 10 days of treatment.
In the reported case, the patient presented with peritonitis due to ileal perforation of uncertain etiology, with subsequent SIRS, septicemia and miliary liver abscess. The bacteria isolated on blood culture was E. coli, which suggests a gastrointestinal source. Septicemia is the most common mechanism of miliary abscess formation [5], and the intestine represents the main gateway for contamination through portal diffusion [4]. A similar case was described in a patient who presented a diverticular perforation of the sigmoid colon complicated by miliary abscess of the liver [7].
CONCLUSION
Miliary abscess of the liver is a rare condition, which requires investigation for immunosuppression or underlying liver disease. Faced with a febrile patient with abdominal pain, an abdominal CT confirms the diagnosis. The blood culture helps to isolate the responsible bacteria. The treatment is based on a prolonged course of antibiotics.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
REFERENCES
- antibiotics
- liver diseases
- hepatic abscess
- abscess
- follow-up
- hepatomegaly
- ileostomy
- immunocompetence
- immunocompromised host
- immunologic deficiency syndromes
- intestinal perforation
- intestines
- pain
- peritonitis
- postoperative period
- togo
- tuberculosis
- diagnosis
- ileum
- liver
- antibiotic therapy
- escherichia coli
- surgical history
- abdominal ct
- blood culture
- rapid diagnosis



