-
PDF
- Split View
-
Views
-
Cite
Cite
Shintaro Kogi, Kei Onodera, Naoko Tsunoda, Tadashi Kawai, Ikuya Miyamoto, Yasunori Takeda, Hiroyuki Yamada, Cystadenoma of the tongue: report of a case with long-term follow-up, Journal of Surgical Case Reports, Volume 2020, Issue 8, August 2020, rjaa269, https://doi.org/10.1093/jscr/rjaa269
Close - Share Icon Share
Abstract
Cystadenoma is a rare benign salivary gland neoplasm characterized by a predominantly multicystic growth pattern. The parotid gland is involved in about 45–50% of cystadenoma cases, with the minor glands of the lip and buccal mucosa being the next most common sites. The tongue is rarely involved; only one congenital case is reported in the literature. Here, we report a 63-year-old man who was referred to our hospital for a nodule on the right edge of his tongue that developed into an elastic soft mass, 4 mm in diameter. It was clinically diagnosed as a benign tumour and removed under local anaesthesia. Microscopically, the lesion was composed of multiple cysts of various sizes and shapes, with or without papillary intraluminal short projections. It was diagnosed as cystadenoma. The postoperative course was uneventful, and we found no evidence of recurrence at the postoperative 14-year follow-up.
INTRODUCTION
Cystadenoma is a rare benign salivary gland neoplasm characterized by a predominantly multicystic growth pattern. It accounts for 4% of all salivary gland neoplasms [1]. Cystadenoma was classified as a separate type of salivary gland neoplasm in 1991 by the World Health Organization (WHO) [2] and further refined into its two major variants of papillary and mucinous cystadenomas in 2005 [3]. Most cystadenomas of the oral cavity are of the papillary type; mucinous cystadenoma is rare. Due to the abolition of these variants, the rare appearance of mucous cells in cystadenoma was documented in the 2017 WHO classification [1]. The parotid gland is involved in about 45–50% of cystadenoma cases, with the minor glands of the lip and buccal mucosa being the next most common sites [1]. The tongue is rarely involved; only one congenital case was reported in the literature [4].
We herein report a rare case of cystadenoma arising in the tongue. To our knowledge, this is the first reported case of cystadenoma of the tongue in an adult.
CASE REPORT
A 63-year-old man was referred to our hospital for treatment of a nodule on his tongue in May 2003. His medical history included Wolff–Parkinson–White syndrome and atrial fibrillation, both of which were controlled adequately by his primary care physician. Physical examination revealed very slight swelling at the right edge of his tongue. The patient reported some spontaneous pain. It was diagnosed as inflammation of the foliate papilla; the patient was followed-up with a gargle prescription. In September 2005, an elastic soft mass, 4 mm in diameter, was observed along the right edge of his tongue (Fig. 1). It was clinically diagnosed as a benign tumour and removed under local anaesthesia. Microscopically, the lesion was composed of multiple cysts of various sizes and shapes, with or without papillary intraluminal short projections (Fig. 2). Many cyst cavities contained eosinophilic fluid. The lesion was well-delineated, but the capsular structure was ill-defined. The stroma was fibrous connective tissue without lymphocytic components. The cystic cavities were lined by a bilayered epithelium composed of luminal columnar cells and basal cuboidal cells. Both luminal and basal epithelial cells were eosinophilic; some clear cells were seen (Fig. 3). Mitotic figures and cellular atypia of epithelial cells were not seen. Immunohistochemically, both luminal and basal cells were CAM5.2+, basal cells were p63+, apical half of the luminal cells were 34βE12+, and the liminal surface was CEA+. The specimen was diagnosed as cystadenoma, based on the histopathological findings.
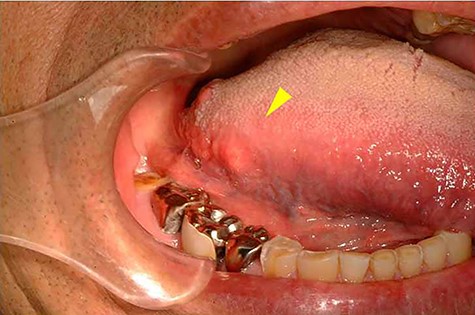
Intra-oral photograph showing the tumour of the tongue (arrowhead).
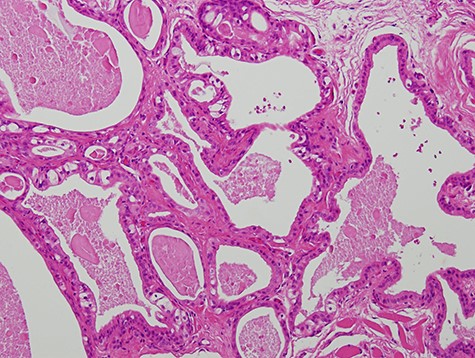
Micrograph showing the lesion composed of multiple cysts of various sizes and shapes (haematoxylin–eosin stain, 100×).
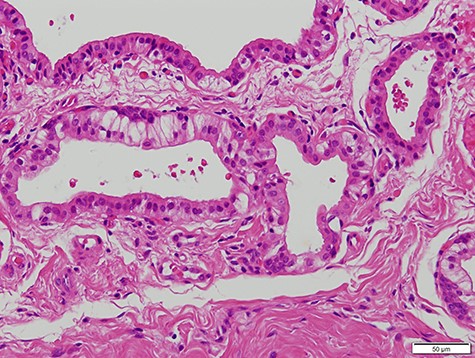
Micrograph showing the cystic cavities lined by a bilayered epithelium (haematoxylin–eosin stain, 200×).
The postoperative course was uneventful, and we found no evidence of recurrence at the postoperative 14-year follow-up.
DISCUSSION
The initial abnormal sign in the present case was slight swelling and pain in the tongue. Pain is an important symptom in oral tumours. In palatal salivary gland tumours, pain and colour alteration were reported to be independent predictors of malignancy [5]. However, the relationship between tumour progression and pain is not obvious; this symptom was merely documented in this report. The benign tumour in this case was not accurately diagnosed at the patient’s first visit, but later, during follow-up, which demonstrates the importance of considering each of a patient’s symptoms when the clinical diagnosis is still unclear.
In this case, image evaluation by magnetic resonance imaging or echography was not performed before resection. Although imaging is usually preferable before resection, this lesion was only 4 mm, and imaging was considered unlikely to confirm any of its properties.
Histopathological differential diagnosis includes ductal ectasia, Warthin tumour, and low-grade mucoepidermoid carcinoma. Ductal ectasia occurs secondarily to salivary obstruction and is characterized by oncocytic metaplasia of the epithelium [6]; however, we observed no obstructive features, such as fibrosis and/or hyalinization of stroma with inflammatory cell infiltration, and clear cells were scattered in the lining epithelium. Warthin tumour has a pronounced lymphoid stroma and bilayered oncocytic epithelium, whereas in cystadenoma, the epithelium is usually not bilayered and lacks lymphoid stroma [7] (however, one case of cystadenoma with unusual prominent lymphoid stroma has been reported [8]). Cystic cavities in the present case were lined by a bilayered epithelium composed of luminal columnar cells and basal cuboidal cells. The stroma was fibrous connective tissue without lymphocytic components. The lack of lymphocytic components thus excluded Warthin tumour. The low-grade mucoepidermoid carcinoma is prominently cystic. Its salient features are infiltrative borders and noncystic epithelial proliferation [7]. However, as the border of our patient’s lesion was well-delineated with no mitotic figures or epithelial cell atypia, our findings did not support malignancy.
Recommended treatment for cystadenoma is complete surgical removal. Recurrence is rare. However, mucinous cystadenoma with malignant transformation [9] and cystadenoma with cervical metastasis have both been reported [10]. Therefore, although 14 years have passed after surgery in the present case, long-term clinical follow-up is scheduled.
ACKNOWLEDGEMENTS
We thank Marla Brunker, from Edanz Group (www.edanzediting.com/ac), for editing a draft of this manuscript.
Conflict of interest statement
None declared.
FUNDING
None.



