-
PDF
- Split View
-
Views
-
Cite
Cite
Yoshiaki Takase, Hiroyoshi Tsubochi, Sachiko Nakano, Tsukasa Suzuki, Toshiteru Nagashima, Osamu Kawashima, Spontaneous pneumothorax in a patient with multiple pulmonary arteriovenous malformations caused by hereditary hemorrhagic telangiectasia: a case report, Journal of Surgical Case Reports, Volume 2020, Issue 8, August 2020, rjaa266, https://doi.org/10.1093/jscr/rjaa266
Close - Share Icon Share
Abstract
Spontaneous pneumothorax occurring in patients with pulmonary arteriovenous malformations (PAVMs) caused by hereditary hemorrhagic telangiectasia (HHT) is extremely rare. We report a case of spontaneous pneumothorax in a PAVM patient. A 26-year-old man with previously diagnosed HHT and multiple small PAVMs presented with chest pain and dyspnea and was referred to our hospital. Chest X-ray showed a left-sided pneumothorax. Computed tomography (CT) showed apical bullae on both sides of the upper lobe. We clarified the location of PAVMs by 3D-CT to avoid the massive bleeding caused by careless grasping of PAVMs and unintentional incomplete resection of the PAVMs during the pneumothorax surgery. Considering the risk of exacerbation, the patient underwent bullectomy of the left upper lobe. The postoperative histopathological examination indicated that the pneumothorax occurred spontaneously in the HHT patient. We should clarify the location of PAVMs to avoid bleeding caused by the grasping of PAVMs during surgery.
INTRODUCTION
Hereditary hemorrhagic telangiectasia (HHT) is a rare autosomal dominant genetic vascular disorder with an estimated prevalence of 1 in 5000–8000 in Japan [1]. To our best knowledge, there is no report of spontaneous pneumothorax occurring in HHT patients. HHT is characterized by multiple arteriovenous malformations (AVMs), in which arteries are directly connected to veins without intermediate capillaries [2, 3]. Although hemothorax has been reported as a complication of pulmonary AVM (PAVM), there is no report of a pneumothorax occurring in PAVM. We report an extremely rare case of pneumothorax in a patient with multiple PAVMs.
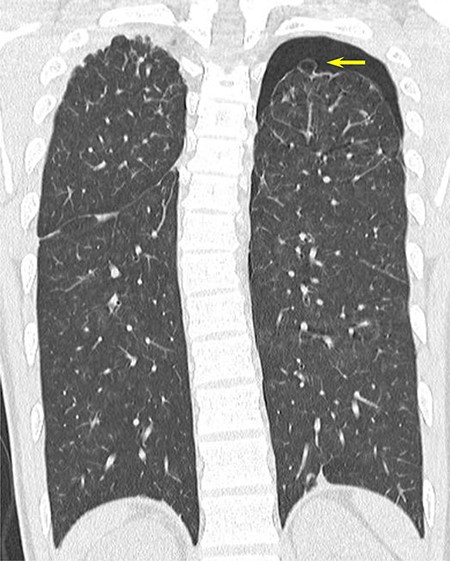
CT scan showing apical bullae on both sides of the upper lobe of the lung and left-sided pneumothorax.
CASE REPORT
A 26-year-old man with no history of smoking complained of chest pain and dyspnea. Chest radiography revealed a left-sided pneumothorax, and he was referred to our institution. He had
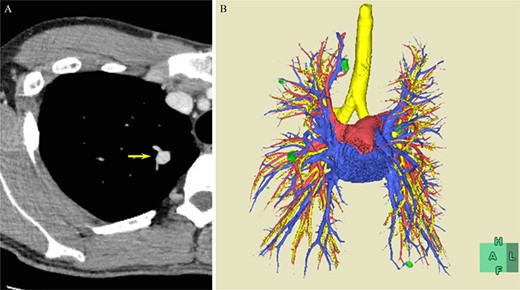
(A) CT scan showing PAVMs in the right upper lung (arrow) and (B) 3D-CT image. Green, PAVM; red, pulmonary artery; blue, pulmonary vein; yellow, trachea and bronchus.
recurrent intermittent epistaxis every few months and was monitored for PAVMs using computed tomography (CT) examinations every 6 months. He had a family history of HHT in his father and grandfather. After systemic examinations, he was diagnosed with HHT because he met the diagnostic criteria, including the presence of PAVM, recurrent epistaxis, and a family history of HHT, although genetic testing was not performed. A chest CT scan showed a left pneumothorax and apical bullae on both sides of the upper lobe (Fig. 1). In addition, a total of six PAVMs (four in the right lung, two in the left lung) were shown on the chest CT (Fig. 2). All PAVMs were located peripherally with the largest one being 3 mm in diameter. No AVM was detected in the brain or abdomen on CT. He was treated conservatively and then pneumothorax was improved. Six months later, the patient complained of cough and was diagnosed with pneumothorax by chest X-ray. To prevent the recurrence of the pneumothorax, the patient was offered video-assisted thoracic surgery. Intraoperatively, apical bullae and multiple telangiectasias were identified under the visceral pleura (Fig. 3). We performed wedge resection of the left upper lobe including the apical bullae. The postoperative histopathological findings of the resected specimen revealed pulmonary bullae (Fig. 4). The postoperative course was uneventful, and the patient was discharged on postoperative Day 2. He underwent catheter embolization for PAVMs in another hospital. His SpO2, which was measured before catheter embolization, was 97% on room air. There was no remarkable change in SpO2 after the intervention. No recurrence of the pneumothorax was observed during a 3-year follow-up.
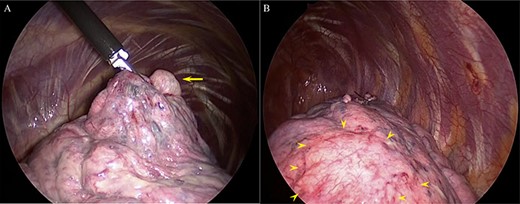
(A) The bullae causing pneumothorax (arrow) and (B) multiple telangiectasias under the visceral pleura (arrowhead).
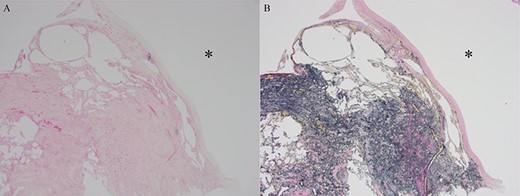
Histopathological findings showing a pulmonary bulla (asterisk in (A) and (B)). (A) Hematoxylin-Eosin stain. (B) Elastica van Gieson stain.
DISCUSSION
Spontaneous pneumothorax occurring in HHT patients is extremely uncommon. It is well known that PAVM can cause hemothorax. Although hemothorax is more common in pregnant women because of increased body fluid and hormonal changes [4], few cases of PAVM rupture have been reported in men [5]. Recently, endovascular treatment will be the first choice for the patients without severe complications such as severe pulmonary hypertension, renal failure and early pregnancy [6]. Formerly, PAVM was treated by only surgical resection. Even now, surgical resection can be selected for the patients who have difficulty to embolize the PAVM or poorly control by hemorrhagic shock [7]. With the development of endovascular techniques, PAVMs with a feeding artery < 3 mm in diameter have become treatable. Thus, currently, in international guidelines concerning HHT, the treatment indication is PAVMs with a feeding artery > 2 mm in diameter [6]. Therefore, we decided to treat PAVM after pneumothorax surgery in our case.
HHT is known to be associated with pulmonary hypertension [8]. However, preoperative echocardiography was not performed in our hospital. After pneumothorax surgery, the patient was referred to a specialist to undergo catheter embolization. The echocardiography performed in the hospital suggested an intermediate possibility of pulmonary hypertension. Thoracoscopic surgery, collapsing one lung and carbon dioxide insufflation can significantly increase pulmonary vascular resistance and pulmonary artery pressures during surgery. Consequently, this may result in right ventricular failure during the procedure. Hence, it is important to note the presence of pulmonary hypertension for anesthetic considerations. Although no problems occurred during surgery at our hospital, preoperative echocardiography should be performed.
The histopathological findings of the resected lung specimen could not indicate an association between the cause of pneumothorax and abnormal blood vessels in our patient. The multiple bullae on the bilateral apical lungs had presented before pneumothorax onset, indicating that the spontaneous pneumothorax occurred with no specified etiology in our patient.
In our case, we should pay attention to massive bleeding caused by damage to the PAVMs during pneumothorax surgery. In a previous report, 3D-CT was useful for determining the location of PAVMs [9]. The 3D-CT can support the surgeons to avoid careless grasping of the PAVMs and unintentional incomplete resection of PAVMs during the pneumothorax surgery. In our case, 3D-CT was useful for determining PAVMs preoperatively PAVMs.
CONCLUSION
We presented a case of spontaneous pneumothorax treated with thoracoscopic surgery in an HHT patient with multiple PAVMs. Histopathologically, there was no association between the development of bullae and AVM or abnormal blood vessels. 3D-CT was useful for determining the location of PAVMs so that we could avoid bleeding caused by the grasping of PAVMs during the surgery.
ACKNOWLEDGMENTS
We thank Editage (https://www.editage.jp/) for editing a draft of this manuscript.
Conflict of interest statement
None declared.
FUNDING
None.
Ethics approval and consent to participate
The publication of this case report was approved by the institutional ethics committee.
Consent for publication
The case report and publication process were explained to the patient, and he granted permission to publish this report.
Authors’ contributions
Y.T., S.N. and T.N. drafted the manuscript. H.T. revised the manuscript critically for important intellectual content. T.S. provided the pathological image. O.K. gave final approval of the version to be published. All authors read and approved the final manuscript.



