-
PDF
- Split View
-
Views
-
Cite
Cite
Preci Hamilton, Peyton Lawrence, Christian Valentin Eisenring, Papillary meningioma: a rare cause of massive supratentorial intracerebral hemorrhage, Journal of Surgical Case Reports, Volume 2020, Issue 8, August 2020, rjaa268, https://doi.org/10.1093/jscr/rjaa268
Close - Share Icon Share
Abstract
Papillary meningioma (PM) represents a very rare histological subtype, which may present with massive intracerebral hemorrhage. Gross total tumor resection results in a lower recurrence rate and mortality. A 69-year-old man had been experiencing headache for 6 months. After exacerbating right frontal headache, he was brought to the emergency room. His Glasgow Coma Scale (GCS) was 11/15 and he had a left-sided hemiparesis. A computed tomography brain scan revealed a massive right frontal intracerebral hematoma with transtentorial herniation. During right frontal craniotomy and blood clot evacuation, a fleshy, pigmented tissue was encountered. Histopathological findings were consistent with PM World Health Organization Grade III. Complete tumor resection, Simpson II was achieved with a second operation. The hemiparesis and GCS normalized subsequently. The diagnosis of PM relies largely on histopathology and is not commonly encountered preoperatively in emergency cases. Staged surgery in this case resulted in a good outcome.
INTRODUCTION
Intracerebral hematoma (ICH) is a common pathology seen by neurosurgeons and mandates rapid treatment. After history taking and clinical evaluation, magnetic resonance imaging (MRI) may be of invaluable importance but may prove time consuming in the event of an emergency.
Papillary meningioma (PM) is a very rare cause of intratumoral hemorrhage and is an aggressive form of an otherwise benign lesion carrying a sinister prognosis of 40% 5-year survival rate [1]. It is usually difficult to diagnose clinically and therefore had largely relied on histopathology and nowadays on molecular pathological profiling since first described by Cushing and Eisenhardt [2].
We present a case of massive intracerebral hematoma, which started out as a diagnostic dilemma but proved to be a hemorrhage into a PM.
CASE REPORT
A 69-year-old hypertensive man was found by his wife on the bathroom floor ~4 hours before referral to the neurosurgery unit at the institution. Before that, he had been complaining of right frontal headache and experienced three episodes of vomiting over the course of the preceding 24 hours. He had been suffering intermittent headache for ~6 months.
Initial assessment in the emergency room revealed a Glasgow Coma Scale (GCS) score of 11/15 (E1 V4 M6), equal and reactive pupils and a dense left hemiparesis—Medical Research Council Grade 1/5 power in both upper and lower limbs. His presenting blood pressure was 162/109 mmHg. He had been taking aspirin with prophylactic indication. Initial non-contrast computed tomography (CT) scan of the brain revealed a massive right frontal intracerebral hematoma with significant vasogenic edema and mass effect as shown in Figure 1.
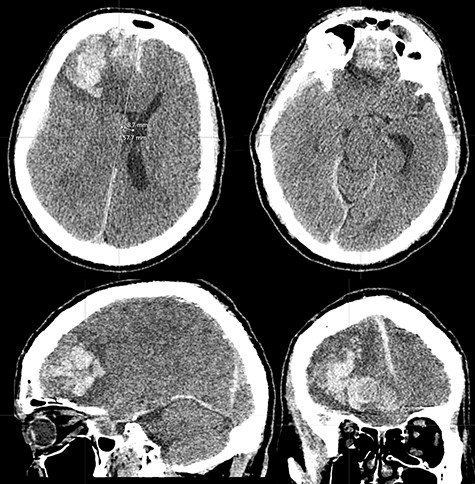
CT brain scan showing massive right frontal ICH causing significant mass effect and transtentorial herniation (superior left and inferior right). There is also moderate vasogenic edema (superior and inferior left). The mass extends to the floor of the anterior cranial fossa (superior right and inferior left).
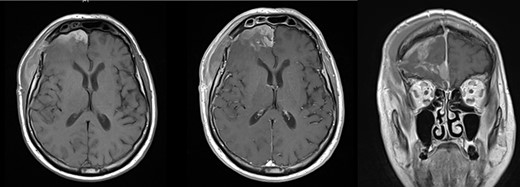
Axial pre- (left) and post-contrast T1-weigted MRI brain (middle) showed relief of the mass effect with correction of the midline shift. Coronal image (right) confirmed residual tumor along the right of the falx cerebri.
The patient was intubated, then osmotherapy (20% mannitol 1 g/kg) and platelet transfusion commenced en route to the hospital. Cerebral CT angiogram on arrival did not reveal a vascular abnormality. He underwent emergency right frontal craniotomy, clot evacuation and debulking of a fleshy, pigmented tissue encountered. There were areas of clearly defined plane between normal and abnormal brain parenchyma; however, this distinction was less evident at other regions. The lesion extended to the anterior cranial fossa floor and was adherent to the anterior third of the superior sagittal sinus (SSS) and falx cerebri. There was neither a vascular abnormality nor was there excessive hemorrhage during surgery. Gross total resection was not targeted in the emergency setting given the intimate relationship of the lesion with the SSS. The evacuated clot and abnormal tissue were sent for histology in 10% formaldehyde. The craniotomy was closed after a pedicled pericranial flap duroplasty was fashioned.
Initial intracranial pressure at closure was 4 mmHg and the patient was monitored in the intensive treatment unit postoperatively. He was successfully extubated and transferred to the open ward within 48 hours after surgery with normal GCS and no focal deficits.
MRI brain was suggestive of meningioma and confirmed residual tumor (Fig. 2). Histopathological findings of perivascular epithelioid cells arranged loosely in sheets with a papillary architecture, immunohistochemical positive staining for vimentin, epithelial membrane antigen (EMA) and progesterone as well as increased Ki67 (5%) fraction, led to a final report of PM World Health Organization Grade III. No other abnormal mass was found on clinical examination.
A reoperation was performed with neuronavigation and microsurgical subpial dissection was able to remove the remaining tumor whilst the anterior third of the SSS was coagulated. Eventually, a Simpson Grade II resection was achieved [3].
The subsequent cerebral MRI found no residual tumor and normal neurological function was preserved. The patient was discharged home in good general condition 12 days after emergency admission.
DISCUSSION
The aim of emergency surgery to control intracranial pressure by evacuating the hematoma was successfully achieved. In retrospect, the extensive degree of edema associated with the hematoma was not in keeping with a vascular bleed but was akin to the slow development of vasogenic edema from a growing tumor.
Although no other tumor deposit was identified on contrast-CT cross-sectional imaging, it revealed that the patient had multiple small pulmonary emboli. This was in keeping with hypercoagulable state of a patient with a neoplasm [4, 5].
There were also reports of epithelioid glioblastoma [6] and perivascular epithelioid cell tumor (PEComa) not otherwise specified [7] presenting in this manner.
Glioblastoma was ruled out because there were no areas of necrosis identified, a lack of glial fibrillary acidic protein and no S100 protein staining on immunohistochemistry (IHC) [6].
PEComas are extremely rare mesenchymal tumors and have been reported to metastasize to the brain [8]. However, HMB-45 was negative thereby eliminating PEComa as a potential diagnosis [8].
A high mitotic rate (Ki67 proliferative marker of 5% labeling) suggested an aggressive tumor and supported the WHO Grade III designation. Therefore, completion resection was justified.
PM represents a very rare histological subtype, which may present with massive ICH, requires immunohistochemistry to make the diagnosis and portends a poor prognosis. The aim of managing these cases of massive intratumoral hemorrhage is hematoma evacuation and complete tumor resection [9].
Hematoma evacuation to release the intracranial pressure was in this case done prior to MRI diagnostics and frozen sections in keeping with the credo: ‘you can always come back to do more on another day’. The chosen staged, elective surgery allowed complete tumor resection and a patient with no focal deficits, which was associated with optimal prognosis.
ACKNOWLEDGMENTS
Authors would like to thank Mr Kaushik Ghosh, Mrs Marcia Donaldson Hugh, Prof. Nihal Gurusinghe and Mrs Elvira Lekka for insightful management guidance and manuscript reviews.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
References
- computed tomography
- cerebral hemorrhage
- headache
- craniotomy
- emergency service, hospital
- glasgow coma scale
- meningioma
- world health organization
- brain
- diagnosis
- mortality
- thrombus
- uncinate herniation
- hemiparesis
- staged operation
- recurrence risk
- tumor excision
- histopathology tests
- symptom aggravating factors
- emergency evacuation



