-
PDF
- Split View
-
Views
-
Cite
Cite
Natsuya Ishikawa, Aina Hirofuji, Shingo Kunioka, Tomonori Shirasaka, Naohiro Wakabayashi, Yuya Kitani, Hiroyuki Kamiya, Impella CP for treatment of left ventricular free-wall rupture after myocardial infarction: Report of a case, Journal of Surgical Case Reports, Volume 2020, Issue 8, August 2020, rjaa263, https://doi.org/10.1093/jscr/rjaa263
Close - Share Icon Share
ABSTRACT
Unloading of the left ventricle (LV) is essential for the treatment of LV free-wall rupture (LVFWR), and it is well-known that the LV can be optimally unloaded with the Impella system. However, there has been no report on applying the Impella system for the treatment of LVFWR. Here, we report a patient with FWR after massive myocardial infarction who was successfully treated with non-suture repair via median sternotomy and implantation of Impella CP (Abiomed, Danvers, MA).
INTRODUCTION
Left ventricular free-wall rupture (LVFWR) after acute myocardial infarction (MI) is a relatively rare but potentially fatal pathology. A sub-analysis of the APEX-AMI trial, in which primary percutaneous coronary intervention (PCI) was performed in 5745 patients, reported that the frequency was 0.52% for LVFWR [1]. Besides of local hemostasis with or without suturing, unloading of the left ventricle (LV) is essential for the treatment of LVFWR, and it is well-known that the LV can be optimally unloaded with the Impella system [2, 3]. However, there has been no report on applying the Impella system for the treatment of LVFWR. Here, we report a patient with LVFWR after massive MI who was successfully treated with non-suture repair via median sternotomy and implantation of Impella CP (Abiomed, Danvers, MA).
CASE REPORT
An Asian male in his 60s complained of sudden chest pain and was referred to a regional hospital. Electrocardiography showed massive ST-elevation in V1-4, and emergency coronary angiography revealed occlusion of the left anterior descending (LAD) artery (Fig. 1a). PCI was successfully performed (Fig. 1b), and IABP was inserted. Maximum value of creatine-kinase was 10 080 U/l, and his left ventricular function was severely impaired with an ejection fraction of 30%. High dosage of catecholamine was administrated and his hemodynamic status gradually recovered; however, he fell into profound cardiogenic shock on post PCI Day 6. Chest X-ray showed significant cardiomegaly (Fig. 2a), and trans-thoracic echocardiography revealed cardiac tamponade.
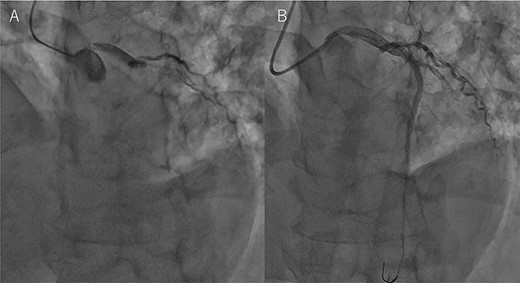
Coronary angiography findings. (A) Pre PCI, the LAD artery was completely occluded. (B) Post PCI, the LAD was recanalized.

Chest X-ray findings. (A) Preoperative, (B) immediately after operation and (C) just after explantation of Impella.
The patient was transferred to our hospital where emergency operation was performed via median sternotomy. Oozing type LVFWR on the anterior wall was found, and was treated with a non-suture technique using TachoSil (Nycomed, Zurich, Switzerland), and without cardiopulmonary bypass. Thereafter, the IABP was removed and Impella CP was inserted percutaneously from the right groin (Fig. 2b). His hemodynamic condition recovered dramatically, and the Impella was removed on postoperative Day 5 (Fig. 2c). The patient was discharged home on postoperative Day 18, and 3 months after the onset of MI, he is doing well.
Written informed consent for publication of this case was obtained from the patient’s wife.
DISCUSSION
To the best of our knowledge, this is the first report on the application of Impella for the treatment of LVFWR.
Traditionally, IABP is widely used for post MI cardiogenic shock including LVFWR [4]. However, since the IABP-SHOCK II trial in which 600 patients with post MI cardiogenic shock were randomly assigned to IABP and control groups showed that there was no significant advantage of IABP [5], Impella has gained attention as an alternative choice for post MI cardiogenic shock.
Impella is an axial flow pump on a pigtail catheter that is placed across the aortic valve to unload the LV by delivering non-pulsatile blood flow to the ascending aorta, making it possible to directly unload the LV. In an animal study, Impella could limit the extent of MI area resulting in improved heart function [6]. Considering the results of the IABP-SHOCK II trial and theoretical advantages of Impella over IABP, Impella appears to be a very attractive modality for cardiogenic shock treatment. However, several studies demonstrated that there was no difference between Impella and IABP in 30-day mortality [7, 8]. Nevertheless, we are in the early stages of assessing in which pathologies Impella could be the optimal modality, and accumulation of further clinical experiences and studies is required.
In this aspect, LVFWR may be one of such pathologies in which Impella could be the better choice for treatment. Okamura et al. [9] reported sutureless repair for post MI LVFWR in 35 patients. In their patients, re-rupture occurred in 17% (6 patients), and four cases (67%) of re-rupture occurred within 24 h after surgery. Their results suggest that effective unloading of the LV in the acute phase post surgery is essential. It is unclear whether IABP was applied to those patients suffering from re-rupture, but it is probable because 13 of the 35 patients (37%) had IABP preoperatively. This implicates that IABP alone may not be sufficient in certain patients with LVFWR, and Impella could be a reasonable alternative for such patients.
In conclusion, a patient with LVFWR after massive MI can be successfully treated by non-suture repair via median sternotomy and implantation of Impella CP. The Impella device may be a reasonable alternative mechanical circulatory support in patients with LVFWR, but further accumulation of clinical experiences and studies are required.
CONFLICT OF INTEREST
None declared.
FUNDING
None.



