-
PDF
- Split View
-
Views
-
Cite
Cite
Alice Rubartelli, Lorenzo Cocchi, Nicola Solari, Ferdinando Cafiero, Michele Minuto, Sergio Bertoglio, Left lower limb fasciitis due to sigmoid colonic perforated diverticulitis: a rare case of colocutaneous fistula, Journal of Surgical Case Reports, Volume 2020, Issue 8, August 2020, rjaa264, https://doi.org/10.1093/jscr/rjaa264
Close - Share Icon Share
Abstract
Up to 25% of patients with acute diverticulitis develop complicated disease. Colocutaneous fistula with lower limb fasciitis secondary to complicated diverticulitis is a rare event. A 71-year-old woman with Class 3 obesity and Type 2 diabetes was admitted to the hospital because of left lower limb fasciitis associated with acute sigmoid diverticulitis complicated by covered perforation. The fasciitis was treated with multiple fasciotomies, antibiotics and hyperbaric oxygen therapy. The patient was readmitted 25 days after discharge because of the formation of a left leg colocutaneous fistula associated with an enterocolic fistula. Patient underwent sigmoid resection with primary anastomosis and ileal loop repair. Three-month follow-up showed fistula healing and absence of symptoms. Fasciitis secondary to acute diverticulitis is a rare clinical scenario. Although our therapeutic strategy was successful, the optimal treatment timing and surgical technique for fasciotomy and colon resection remain to be assessed.
INTRODUCTION
Fistula formation in diverticular disease occurs in 1–12% of patients with acute diverticulitis. Colovesical fistulas are most common, followed by colovaginal and ileocolic fistulas [1–3]. Fasciitis as the first presentation of diverticulitis complicated by colocutaneous fistula is extremely rare and consequently the optimal management of this clinical condition is not yet established. Only few case reports regarding individual patients have been published [4–9].
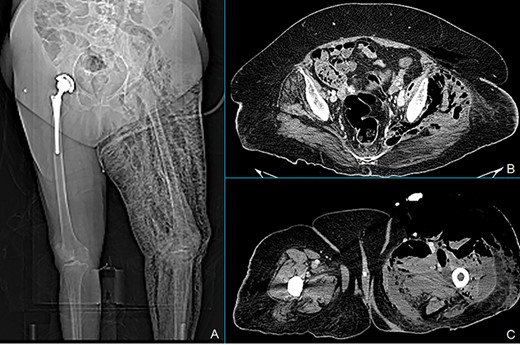
Total body X-ray shows marked left leg emphysema (A). CT scan of the lower abdomen showing covered posterior sigmoid perforation, sigmoid thickening and retroperitoneal collections (B). Marked air and fluid collections in medial and anterolateral compartment of the left leg at the CT scan (C).
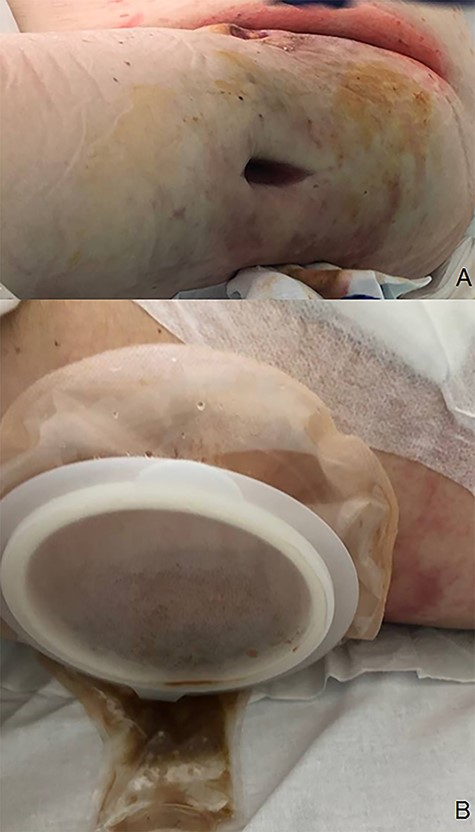
Left leg lateral fasciotomy producing fecal material (A). Ostomy bag device used for colocutaneous fistula managing (B).
CASE REPORT
We report a case of a 71-year-old woman with Class 3 obesity and Type 2 diabetes. The patient initially came to the emergency room for abdominal pain, fever (38.5°C) and swelling of the left lower limb. The blood tests showed a neutrophilic leukocytosis with white blood cells (WBC) 15 700 cells/mmc, neutrophils 13 800 cells/mmc, C-reactive protein (CRP) 303 mg/l and serum glucose 275 mg/dl. At the physical examination, the abdomen was soft with lower left quadrant tenderness, and the left lower limb was painful and warm with marked edema starting from the inguinal region. The patient was hemodynamically stable. Computed tomography (CT) scan of the abdomen extended to the lower limbs (Fig. 1) revealed the presence of air and fluid retroperitoneal collections, extending through the posterior abdominal wall muscles until the medial and anterolateral compartment of the left leg. Besides, thickening of the sigmoid wall with covered perforation was detected. Clinical and radiological findings were consistent with extensive gangrenous fasciitis possibly secondary to perforated diverticulitis. Wide-spectrum antibiotic therapy with meropenem and vancomycin was started and urgent fasciotomies were performed on the anterior, medial and lateral sides of the left leg. The patient was also treated with hyperbaric oxygen therapy and referred to the intensive care unit (ICU). A cultural test showed a polymicrobial infection of Klebsiella pneumoniae, Enterococcus faecalis and Candida albicans. Blood cultures were positives for Staphylococcus epidermidis. According to these findings, the antibiotic therapy was implemented by adding fluconazole and the hyperbaric therapy was stopped. The first postoperative course was uneventful. In postoperative Day (POD) 8, a CT scan showed a reduction of collections both in the retroperitoneum and in the left leg prompting the discharge of the patient from ICU. At that moment, we decided not to treat the diverticulitis surgically, according to the recent Consensus Statement of the European Association for Endoscopic Surgery and Society of American Gastrointestinal and Endoscopic Surgeons. In POD 16, since blood tests were completely normalized, physical examination of the abdomen was negative and surgical incisions were dry and clean, the patient was transferred to the rehabilitation unit. After 37 days from surgery, the patient was readmitted to our unit because of the occurrence of fever and the formation of a fistula at the site of the lateral fasciotomy producing fecal material (Fig. 2). The CT scan revealed marked improvement of abdominal and limb conditions, with a reduction of the pericolic abscess, collections and edema of the left leg (Fig. 3). Lab tests showed WBC 7800 cells/mmc, CRP 183 mg/l. Although CT scan findings showed improvement, the clinical evidence of colocutaneous fistula prompted us to surgery. Intraoperative findings confirmed acute diverticulitis with posterior covered perforation and retroperitoneal fistula. An enterocolic fistula was also detected. There was no contamination of the peritoneal cavity; so we performed sigmoid resection with primary mechanical end-to-end anastomoses without proximal diversion and ileal loop repair. Two drain tubes were placed both in the abdominal cavity and through the lateral fasciotomy. No early or late severe postoperative surgical complications were observed. In POD 4, the patient returned to normal bowel function and started oral refeeding. Abdominal and left leg drain tubes were respectively removed in PODs 5 and 7. An episode of fever (39.3°C) occurred in POD 9 and was attributed to candida infection and treated with antifungal therapy and central venous catheter removal. In POD 27, the patient was finally discharged in good clinical condition with normal lab tests and left leg wound re-epithelialization.
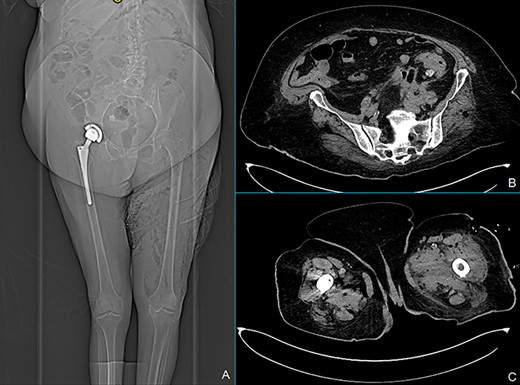
CT scan at the readmission: X-ray showed marked improvement of left leg emphysema (A), a decrease of pericolic abscess (B) and marked reduction of left leg collections (C).
DISCUSSION
Diverticular disease is a common clinical condition in western countries. Up to 25% of patients with acute diverticulitis develop complicated disease [1–3]. However, fasciitis of the limb with colocutaneous fistula is a rare event [4–9].
Therefore, the optimal management strategy is not well defined. Fasciitis of the limbs is a life-threatening condition that requires intensive medical treatment and quite always surgical fasciotomy. On the other hand, colic covered perforation without widespread peritonitis may not require urgent surgery and can be managed medically. In our patient, the massive infective involvement of the left leg mandated urgent fasciotomy, whereas the favorable evolution of the clinical and radiological abdominal signs prompted us to defer surgical repair of the colic perforation. Nevertheless, the evolution toward a colocutaneous fistula must not be underappreciated and the patient should be strictly monitored. In case of occurrence of such complication, surgical treatment becomes unavoidable. In the rare occurrence of colocutaneous fistula, there is no consensus about the surgical strategy regarding the type of colonic resection. In our patient, we performed a sigmoid resection with primary mechanical end-to-end anastomoses without proximal diversion because, quite unexpectedly, we found the peritoneal cavity not contaminated.
In our patient, as reported by others, the severity of fasciitis was not related to the abdominal involvement. Only a few reports are present in literature, and there is no unanimous consensus about the treatment and the timing of surgery.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.
ETHICAL STATEMENT
All authors declare that the manuscript has not been submitted to more than one journal for simultaneous consideration and it has not been published previously (partly or in full). No data have been fabricated or manipulated (included images) to support the conclusions. The paper is not split up into several parts to increase the quantity of submission and submitted to various journals or to one journal over time. No data, text or theories by others are presented as if they were the author’s own.



