-
PDF
- Split View
-
Views
-
Cite
Cite
David Beaton Comulada, Saul Hernández-Rodríguez, Lenny Rivera, Charles Zierenberg, Luis Lojo-Sojo, Anterior tibialis artery pseudoaneurysm after minimally invasive plate osteosynthesis in the proximal tibia: a case report, Journal of Surgical Case Reports, Volume 2020, Issue 8, August 2020, rjaa168, https://doi.org/10.1093/jscr/rjaa168
Close - Share Icon Share
Abstract
Tibial plateau fractures are common fractures associated with high-energy trauma. The treatment of these fractures remains a challenge today. Recent management of fractures has moved from open surgery toward minimally invasive surgery to reduce complications and improve functional outcomes. Nevertheless, such a minimalistic approach makes visualization of neurovascular structures difficult, placing them at risk. We report the case of a 39-year-old male who developed a pseudoaneurysm of the anterior tibial artery following minimally invasive plate osteosynthesis of the right proximal tibia. Diagnosis was made through noninvasive duplex ultrasound and was referred to endovascular service. Understanding of the anatomy of the surgical site is vital to minimize complications. In addition, proper postsurgical patient evaluation is important to monitor the insurgence of such complications.
INTRODUCTION
The treatment of complex tibial plateau fractures remains today a clinical challenge. These fractures are often classified using the Schatzker or AO classification. Treatment options vary from closed nonoperative management to operative management, such as external fixation, intramedullary nailing and open reduction internal fixation with plates and screws. Operative management has transitioned from open surgery toward minimally invasive surgery in an attempt to reduce complications and improve functional outcomes [1]. Minimally invasive plate osteosynthesis (MIPO) has become an adequate treatment option for periarticular and long-bone fractures [2]. The principle of MIPO consists of indirect fracture reduction and maintenance of fracture biology, soft-tissue and stable plate fixation [3].
There are limited studies evaluating vascular injury during tibia fixation. Most studies consist of cadaveric studies, and few case reports in literature describe vascular complications [1, 2, 4–8]. We report a case of a patient who underwent MIPO of a tibial plateau fracture and developed a pseudoaneurysm of the anterior tibialis artery (ATA).
CASE REPORT
A 39-year-old male pedestrian was injured in a motor vehicle accident and then transferred to our emergency room on the same day of injury. Patient was stable after the accident and medical history was noncontributory. Physical examination of the right leg demonstrated considerable soft-tissue swelling around the knee and proximal tibia deformity and no signs of neurovascular injury. Imaging revealed a Schatzker type VI tibial plateau fracture (Fig. 1). Computer tomography angiography revealed no vascular damage. The leg was immobilized with a splint, adequate analgesia was prescribed and the patient was admitted to ward.

Radiographic views demonstrating a complex proximal tibia fracture of the right leg.
During hospital stay, patient demonstrated no deteriorating signs. External fixation due to continued swelling of the knee was performed with informed consent of the patient. Postsurgical evaluation was uneventful. Patient was discharged on second postoperative day with proper analgesia and anticoagulation therapy (enoxaparin 40 mg SQ daily for 14 days). At the 2-week follow-up, the external fixator was in place, and there were no concerning physical exam findings. Thus, patient was scheduled for removal of external fixator followed by internal fixation of the proximal tibia.
Three weeks after initial injury, minimally invasive osteosynthesis was performed using a 12-hole precontoured proximal lateral tibia plate (I.T.S., GmbH, Graz/Austria). Patient was draped and placed in supine position under spinal anesthesia: nonsterile pneumatic tourniquet was placed and inflated to 350 mmHg. The external fixator was removed, and an anterolateral incision was made on the right proximal tibia for fracture fixation. Insertion guide and plate were inserted between anterior tibialis muscle and periosteum. Insertion of screws was performed with the aid of C-arm fluoroscopy (for proper screw placement). After tourniquet was deflated, surgical incision was closed with sutures. During the procedure, no signs of brisk bleeding or damage to neurovascular structures were observed. Immediately after the procedure, the patient exhibited symmetrical palpable peripheral pulses of dorsalis pedis and posterior tibialis arteries. Postsurgical radiographic images revealed excellent fracture reduction and alignment (Fig. 2). Hospital stay was uneventful, and patient was discharged home the next day with pertinent postoperative management instructions.

(A) Anteroposterior and (B) lateral views of the right tibia following minimally invasive percutaneous osteosynthesis. Images reveal proper alignment and fracture reduction.
Two-week postoperative follow-up demonstrated a clean wound and intact peripheral pulses. At the 6-week follow-up, clinical evaluation revealed a right mid leg anterolateral pulsating tender mass initially noticed by the patient 8 days prior to this visit. Patient stated no recent trauma. Noninvasive duplex ultrasound performed revealed a 3.4 × 2.7 cm pseudoaneurysm at the ATA (Fig. 3). Patient was referred to endovascular service for recommendations and management. Alternatives such as observation and ultrasound-guided compression or percutaneous ultrasound-guided thrombin injection were discussed with the patient if pseudoaneurysm did not spontaneously thrombose after 1 month. Patient was ultimately managed conservatively since he remained asymptomatic, and latest ultrasound revealed spontaneous resolution by 3 weeks of diagnosis.
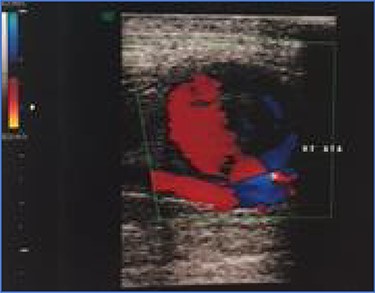
Noninvasive duplex ultrasound demonstrating a 3.4 x 2.7 cm pseudoaneurysm at the anterior tibialis artery.
DISCUSSION
MIPO is now considered an adequate treatment option with the main goal of reducing soft-tissue disruption and devascularization while preserving fracture biology [1]. Literature reports good functional outcomes with this treatment method in the management of tibia fractures [3]. However, the less-invasive nature of the procedure can make visualization of neurovascular structures and direct fracture reduction difficult [3]. In our case, the patient developed a pseudoaneurysm after undergoing MIPO due to a high-energy tibial plateau fracture (Schatzker type VI). To our knowledge, this is the first case reported in the literature with this clinical presentation.
There have been previous reports of pseudoaneurysm development during management of the tibia. Injury to the anterior tibialis system has occurred during placement of an intramedullary nail (IMN). Inamdar et al. reported this complication when placing the proximal or distal interlocking screw of the IMN [6]. Reports of pseudoaneurysm after MIPO are limited, with the majority of cases reported occurring at the distal tibia [8]. The only report of an injury to the anterior tibialis system after MIPO of a proximal tibial plateau fracture was made by Gary et al. [2]. They described an arterial injury during screw placement that was successfully managed intraoperatively; however, it did not develop a pseudoaneurysm.
In our case, the patient’s pseudoaneurysm was found 6 weeks after surgery. The most likely cause was injury with placement of the percutaneous screw during the surgery. Injury to the arterial wall causes an acute local hemorrhage that consequently leads to a tamponade effect by the surrounding tissues. It becomes clinically detectable by the surgical staff when the blood clot eventually liquefies resulting in the formation of fibrous capsule surrounding the artery (a pseudoaneurysm) [6]. The ATA is a branch of the popliteal artery that emerges at the lower end of the popliteus muscle. It courses anteriorly and lies on the interosseous membrane medial to the fibular neck. There are variants to the ATA as observed in multiple cadaveric studies [1, 4, 5, 9]. A high-origin ATA is defined as an ATA that arises proximal to the popliteus, above the middle portion of the posterior surface of the popliteus with a prevalence of 1.9–4.2% [9]. A cadaveric study displayed that the neurovascular bundle of the tibia crosses from the posterior compartment to the anterior compartment between 40 and 110 mm proximal to the tibia ankle [10]. However, Heidari et al. determined that the anatomic safe zone can be as little as 27 mm distal to the lateral tibial plateau [5]. The management for a pseudoaneurysm is multiform [6]. It includes external compression, ultrasound-guided compression, ultrasound-guided thrombin injection, percutaneous endovascular coil embolization or percutaneous endovascular stenting [7]. Surgical excision of the pseudoaneurysm can be performed with additional ligation of the artery or restoration of blood flow through an end-to-end anastomoses or vein graft [6]. Decision-making ultimately depends on the treating physician and thorough assessment of the anatomic location and arterial competency of the pseudoaneurysm.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
The authors have not received grant support or research funding for this study.



