-
PDF
- Split View
-
Views
-
Cite
Cite
Mohamed Hafedh Saadi, Ahmed Saadi, Marouene Charkoun, Cyrine Saadi, Zinet Ghorbel, Marwa Bouafif, Mariem Ksantini, Sofiene Sayari, Abderazek Bouzouita, Amine Derouiche, Riadh Ben Slama, Haroun Ayed, Mounir Ben Moussa, Soumaya Rammeh, Mohamed Chebil, Prostatic cystadenoma presenting as a large multilocular pelvic male mass, Journal of Surgical Case Reports, Volume 2020, Issue 8, August 2020, rjaa244, https://doi.org/10.1093/jscr/rjaa244
Close - Share Icon Share
Abstract
Multilocular cystadenoma are benign lesions located most commonly between the rectum and the bladder. Their presence manifests as obstructive or/and irritative lower urinary tract symptoms or transit disorders. Computed tomography scan and magnetic resonance imaging may help to establish the diagnosis. Surgery is the established treatment standard, with a high risk of recurrence in case of incomplete excision of the lesions. Here we report a case of 59-year-old man presenting with an acute urinary retention due to a giant multilocular prostatic cystadenoma treated by complete excision. The diagnosis has never been suspected before surgery and has been confirmed histologically after complete excision.
INTRODUCTION
Multilocular cystadenomas of the lower genitourinary tract are benign lesions [1–6] that originate from the prostate, less frequently from the seminal vesicles or cowper’s glands. Typically, it presents as multilocular cysts that varies in size from one patient to another and located most commonly between the rectum and the bladder [3]. Their presence manifests as obstructive or/and irritative LUTS or transit disorders [1–3]. Surgery is the established treatment standard [1–7].
Hereafter, we report a case of a 59-years-old man with a giant multilocular cystadenoma of the prostate, initially presenting with an acute urinary retention. The diagnosis was never been suspected before the pathological examination results.
CASE REPORT
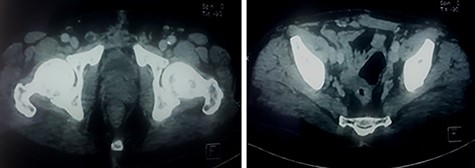
A 59-year-old patient presented at the emergency department with an acute urine retention. As a past medical history, the patient suffered from chronic hypogastric pain with LUTS and constipation over a period of 6 months. The clinical examination revealed a distended bladder that required transurethral bladder catheterization. The digital-rectal examination showed a bulging pelvic mass in the rectum, the prostate has not been palpated. The blood analysis revealed an elevation of creatinine level to 123 μmol/l with hyperleukocytosis. Prostate-specific antigen (PSA) was within normal range and urine culture was negative. Abdominal and pelvic Computed tomography (CT) scan was performed and showed a multilocular heterogeneous cystic mass in the rectovesical and supravesical spaces, measuring 13 × 10 × 9 cm, compressing the bladder and the two ureters with bilateral major upper tract dilation. The cystic mass had many septa of different thickness mildly enhancing after contrast administration (Fig. 1). There were no nodular solid enhancing components or evident signs of lymphadenopathies or metastatic lesions.

CT scan showing pelvic multilocular heterogeneous cystic mass with many septum mildly enhancing after contrast.
A hydatic cyst was suspected but hydatic serology was done twice and was negative. We completed in the first place by a urethrocystography on which we notice the presence of a 12-cm mass projecting on the bladder area (Fig. 2). And to better and further characterize this cystic formation, a pelvic magnetic resonance imaging (MRI) was performed, concluding the presence of a 13 × 10 cm supra-rectal and retro-vesical multilocular cystic formation of heterogeneous signal, with the presence of liquid level in some loci, having a T1 hypersignal (Fig. 3) and T2 hypo signal evoking a hematic content having a thin wall increasing after injection of gadolinium, the whole evoking either a hemorrhagic cystic retro-peritoneal mesothelioma or cystic lymphangioma.
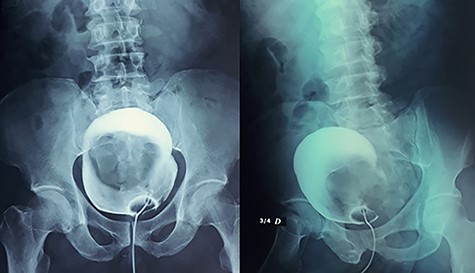
Presence of a 12-cm mass projecting on the bladder area in the cystography.
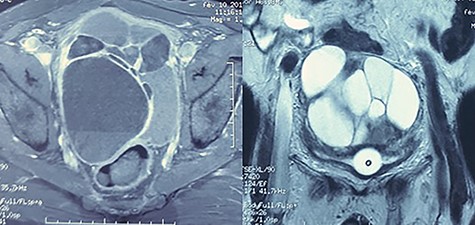
MRI: multilocular cystic formation of heterogeneous signal, with the presence of liquid level in some loci, having a T1 hypersignal and T2 hyposignal.
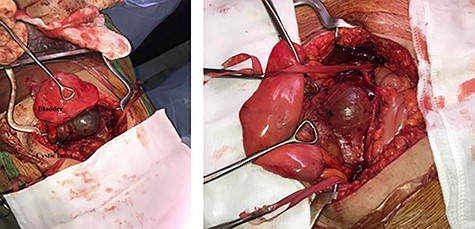
At first, the patient had a cystoscopy which was difficult to perform (no identification of the ureters due to an inflammatory mucosa). Then, a midline incision was done, the exploration found a large pelvic cyst under the peritoneum pushing the bladder forward (Fig. 4), the ureters that are dilated and the rectum. We performed a complete dissection of the cystic mass with accidental bladder wound, which was repaired. The dissection of the anterior wall of the rectum resulted in a 1-cm rectal leak sutured and protected by a left iliac colostomy.
The immediate postoperative follow-up was simple with restoration of the transit on Day 2, an exit on Day 7 postoperation. The bladder catheter was removed after 10 days. The control creatinine level on Day 15 was 75 μmol/l.
In pathological examination, the gross pathologic specimen was a 10 × 9 × 4 cm mass containing multiple varied-size cysts. Histologically, the tumor was composed of acini, dilated glandular structures and cyst lined by prostatic-type epithelium set in a hypocellular stroma. No atypical features or mitosis was noted in neither the glandular nor the stromal components of the mass (Fig. 5). These lesions matched with a multilocular prostatic cystadenoma.
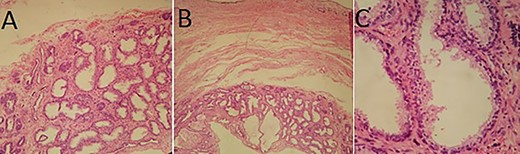
Pathological examination: (A and B) cystic wall containing numerous acini and dilated glandular structures (HES×10 and ×4); (C) Acini and cysts lined by prostatic-type epithelium (HES×20).
The patient was seen on Day 15, 1 month, 3 months, 9 months postoperatively. The control CT scans made at 3 and 9 months postoperatively had shown no abnormalities without any residual mass (Fig. 6).
Control CT scan at 9 months postoperatively: the bladder and prostate are normal in appearance and there is no residual mass.
DISCUSSION
Prostatic adenomas are rare benign prostatic tumors having the potential to attain large dimensions. The clinical presentation in all patients is similar to benign prostatic hyperplasia with frequently lower urinary tract symptoms [1–3]. Other symptoms like defecation problems may occult the urinary symptoms due to rectal compression by the mass [2].
In the literature, the age of presentation is variable between 23 and 80 years old [1–7]. Physical examination may find some signs of obstruction (distended bladder, tenderness of the lumbar region and fecal impaction) and an enlargement of the prostate is typically seen by digital rectal examination. PSA value may or may not be elevated [1]. CT and in particular MRI can provide information on a large cystic process originating or not from the prostate (the origin is rarely determined by the imaging) [1,3–6]. In the CT scan, the lesion frequently present as a giant multiloculated mass composed of variable-sized cysts, with some septations enhancing after contrast administration. In some cases, solid enhancing areas can be found within the lesion posing some diagnostic difficulties [1–4]. However, the most distinguish feature is that it present as well-defined non-infiltrative masses of indolent growth [3–5]. In fact, in the presented case, the lesion had sharp marinated borders, appearing to push the adjacent structures away and not invading into them.
Differential diagnosis of prostatic cystadenoma may include the phylloid variant of atypical prostatic hyperplasia, prostatic leiomyoma, prostatic sarcoma, cystic prostatic carcinoma, infection (hydatic cysts, echinococcosis or cavitary prostatitis with or without abscesses), pelvic mesothelioma, lymphangioma, peritoneal inclusion cyst and teratomas [1–6].
Complete surgical excision is the optimal treatment option even if it may be very difficult due do adherences with surrounding structures [1–6]. Incomplete excision can lead to tumor recurrence [1–6]. Surgery complications are bladder and rectum perforation or vascular complications which may be fatal for the patient. That’s why endoscopic treatment (TURP) has been proposed for some recurrent cases of small prostatic cystadenomas [7]. One case reported that a treatment with gonadotrophin-releasing hormone antagonist can be effective for recurrent multilocular prostatic cystadenomas [8]. In fact, some studies reported that the treatment with Luteinizing Hormone-Releasing Hormone (LHRH) antagonists alone, or as neoadjuvant or adjuvant may have showed success apparently. But since it is often difficult to differentiate a prostatic cystadenoma from a cystic prostate cancer preoperatively, it has been admitted that the lesion in these cases may in fact be a cystic prostate cancer that was wrongly diagnosed as prostate cystadenoma or rather a combination of prostate cyst adenoma and cystic prostate cancer, which explains the successful treatment by LHRH antagonists [9]. That is why we strongly believe that the treatment of choice for giant multilocular prostatic cystadenoma is complete surgical excision.
In conclusion, multilocular prostatic cystadenoma may be a rare entity but every physician should be aware of this condition when confronted with large pelvic masses of unknown history or that possibly maybe related to the prostate. Surgery is often necessary in most of the cases and the excision must be complete in order to avoid recurrence and regrowth of masses.
CONFLICT OF INTEREST STATEMENT
None declared.
CONSENT
Authors declared that they received written consent from the patient to publish this case report.



