-
PDF
- Split View
-
Views
-
Cite
Cite
Leah Sukri, Laura DiChiacchio, Philip J Wasicek, Stephen M Kavic, Small bowel necrosis and perforation due to sodium polystyrene sulfonate in the setting of graft versus host disease and fulminant Clostridium difficile infection, Journal of Surgical Case Reports, Volume 2020, Issue 8, August 2020, rjaa253, https://doi.org/10.1093/jscr/rjaa253
Close - Share Icon Share
Abstract
Gastrointestinal injury is a common adverse event associated with use of sodium polystyrene sulfonate (SPS), tradename Kayexalate. Risk factors for SPS-mediated gastrointestinal necrosis include chronic kidney disease, solid organ transplant recipiency and recent surgery. This report presents a patient with past medical history significant for acute myeloid leukemia (AML) complicated by graft versus host disease (GvHD) and Clostridium difficile colitis who initially presented with small bowel obstruction. She was taken to the operating room and her small bowel pathology was significant for transmural necrosis with SPS crystals in the granulation tissue, despite last receiving SPS over a year ago. Previous mucosal damage should be considered as a risk factor for SPS-mediated injury and the effects of this medication may occur longer than previously thought.
INTRODUCTION
Sodium polystyrene sulfonate (SPS) is commonly used to manage hyperkalemia by increasing potassium excretion through the gastrointestinal (GI) tract. Although it has been used since the 1950s, there have been rising reports of SPS causing fatal GI injury. This includes intestinal ischemia, necrosis, ulceration and perforation [1]. In this report, we present an unusual case of small bowel necrosis associated with SPS in a patient with stricturing graft versus host disease (GvHD) and recurrent Clostridium difficile colitis.
CASE REPORT
A 60-year-old female presented with a 1 day history of sharp abdominal pain with vomiting. She has a previous history of acute myeloid leukemia (AML) complicated by biopsy-proven GvHD in the GI tract following a matched unrelated donor allogenic hematopoietic stem cell transplant (HSCT) 3 years prior. On biopsy at that time, her stomach, cecum and colon all showed increased apoptotic activity with apoptotic crypt abscess, while her ileum showed complete mucosal denudation. Her home medications included amoxicillin, tacrolimus, budesonide and an alpha-1 proteinase inhibitor. She was most recently hospitalized 1 month prior for 4 days for small bowel obstruction (SBO) that was medically managed.
Upon presentation, she was afebrile and had a soft bowel movement hours prior to arriving in the emergency department. Her abdomen was soft with mild diffuse tenderness and distention. Significant laboratory values included a white count of 10.8 K/μl, hemoglobin 8.0 g/dl, potassium 3.3 mmol/l, blood urea nitrogen (BUN) 27 mg/dl, creatinine 0.77 mg/dl and lactic acid 2.0 mmol/l. An abdominal/pelvic computed tomography (CT) scan was performed, which revealed SBO at the level of the distal ileum and diffuse colitis. The next day, she went into fulminant sepsis with a fever of 38.9°C, lactate of 2.2 mmol/l and systolic blood pressure in the 80s despite infusion of 3 l of crystalloid and vasopressor support. She was found to be positive for Clostridium difficile (C diff) and was taken to the operating room for an emergent laparotomy with the presumed diagnosis of fulminant C diff colitis.
Fifty centimeters of diseased ileum that consisted of multiple strictures and adhesions was resected and a double barrel ileostomy was formed for antegrade colonic vancomycin lavage. The patient had an uneventful recovery. Pathology of the specimen revealed necrosis in the small bowel segment along with a full thickness ulcer with granulation tissue, consistent with an ischemic type injury pattern. SPS crystals were identified within the granulation tissue despite no record of SPS administration more recently than 1 year prior for hyperkalemia (Fig. 1).
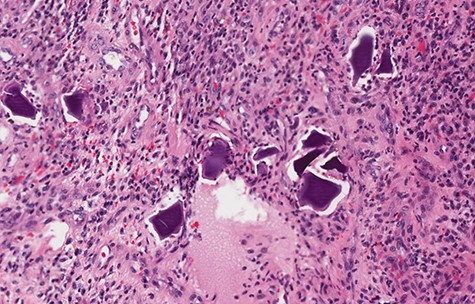
Small bowel biopsy revealing SPS crystals in intestinal mucosa with inflammatory changes.
DISCUSSION
Although our patient has several reasons to have sustained intestinal injury, her tissue pathology is consistent with SPS-mediated necrosis. We find this case unusual given the extended time between SPS administration and bowel injury. Furthermore, as our patient does not have the usual risk factors associated with this injury, we must consider what put this patient at an increased risk.
In recent years, SPS use has been out of favor due to its dubious efficacy in treating hyperkalemia, and its morbid adverse events [1]. Patients with SPS toxicity often present with abdominal pain, distention, GI bleeding, diarrhea, nausea and vomiting. Harel et al. [1] conducted a systematic review of SPS-mediated GI injury and noted that a majority of injury occurs in the colon, while 10% of cases occurred in the small intestine. Histopathologic findings include transmural necrosis, ulceration, erosion and pseudo-membrane formation, while SPS crystals are pathognomonic [1]. Risk factors for SPS-mediated injury include a history of kidney disease, solid organ transplant or recent surgery [1].
On the other hand, GvHD occurs in many patients with allogeneic HSCT. It is believed that antigen presenting cells and alloreactive donor T cells mediate damage against various recipient tissues [2]. Acute GvHD in the GI tract generally presents as voluminous diarrhea, nausea, anorexia or bleeding. Histology often displays patchy ulceration, crypt abscess and apoptotic bodies in the crypts [2]. Chronic GvHD in the gut presents with weight loss, esophageal web or strictures. Bowel obstruction occurs most often in patients who have not previously responded to medical therapy [3]. Tissue histology generally shows diffuse inflammation and reactive epithelial change, not necrosis.
There is an established relationship between GvHD and Clostridium difficile infections, with almost 85% of patients who were diagnosed with GvHD having a previous C diff infection [4]. There is a 12–27% rate of C diff infection in patients with allogeneic HSCTS [4]. C diff colitis can present as profuse watery diarrhea, but has occasionally been associated with ileus. In most severe cases, fulminant colitis can occur leading to toxic megacolon, colonic perforation and death.
Our patient with transmural necrosis on small bowel biopsy may have been triggered by a variety of factors that includes past SPS use, GvHD and Clostridium difficile colitis. Although she does not have the risk factors commonly associated with this SPS-mediated GI injury, she does have an increased susceptibility for intestinal damage. Her previous intestinal injury caused a loss of mucosa in her ileum. She was also on chronic immunosuppressive and steroid treatment, which impairs tissue integrity and wound healing. Her recurrent SBO and Clostridium difficile colitis may have contributed to tissue necrosis due to underlying ischemia and ileus. It is unclear what the precipitating factor for the patient’s small bowel necrosis is, but the biopsy of the specimen is consistent with SPS-mediated damage due to the presence of crystals and transmural necrosis.
To our knowledge, there are few reported instances of SPS-induced damage in patients without kidney disease. Outside of this predominant risk factor, we must consider previous mucosal damage as another potential risk factor for SPS-associated intestinal necrosis, in this case, her underlying GvHD and recurrent Clostridium difficile colitis. Furthermore, the timing of the injury in our case appears to be much longer than what has been documented in the literature, which may indicate that SPS has longer lasting effects than previously thought. We believe that this case report is interesting and prompts further research into the adverse effects of SPS.
CONFLICT OF INTEREST
The authors have no conflicts of interest to declare.
FUNDING
None.
REFERENCES
- leukemia, myelocytic, acute
- small bowel obstruction
- kidney failure, chronic
- clostridium difficile infections
- graft-versus-host disease
- granulation tissue
- intestine, small
- necrosis
- operating room
- surgical procedures, operative
- medical history
- mucous membrane
- pathology
- surgery specialty
- transplanted organ
- sodium polystyrene sulfonate
- gastrointestinal tract injuries
- pseudomembranous colitis
- small bowel necrosis
- transmural
- adverse event
- crystal structure



