-
PDF
- Split View
-
Views
-
Cite
Cite
Mairead Kelly, Georgios Oikonomou, Chrysostomos Tornari, Imran Ahmad, Andrea Bille, Jean-Pierre Jeannon, Asit Arora, Single-session, dual-site robotic surgery for synchronous primary malignancies of the oropharynx and thorax, Journal of Surgical Case Reports, Volume 2020, Issue 8, August 2020, rjaa258, https://doi.org/10.1093/jscr/rjaa258
Close - Share Icon Share
Abstract
Single-session, dual-site robotic surgery for synchronous malignancies is not widely reported. To our knowledge, there are no previous reports of transoral robotic surgery (TORS) and robot-assisted thoracic surgery (RATS) in a single sitting. A 49-year-old male presented with a neck lump. Biopsies and imaging proved synchronous primaries of the tonsil and lung. The morbidity of primary dual-site chemoradiotherapy, or open surgery, presented a management challenge. We therefore opted for sequential robotic resections, in a single sitting. The patient was discharged on Day 6 post-operatively and was able to start radiotherapy less than 3 weeks post-operatively. Undertaking TORS and RATS in a single sitting is feasible and safe. This approach allowed fast-tracking of adjuvant oncological therapy, arguably conveying the greatest chance of cure. We detail the rationale and utility of this novel approach and describe the surgical and anaesthetic challenges of two teams undertaking sequential robotic procedures in a single sitting.
INTRODUCTION
Transoral robotic surgery (TORS) is a valuable treatment for oropharyngeal squamous cell carcinoma, avoiding the need for a jaw split and tracheostomy [1]. Robot-assisted thoracic surgery (RATS) is popular for major lung resections and mediastinal mass excisions, reducing the need for thoracotomy [2] and time to adjuvant therapies [3].
Robotic surgery on two anatomical sites, in a single sitting, remains uncommon. A literature review found 22 such case reports. The vast majority were abdominal or pelvic, undertaken by a single surgical team [4, 5]. Cases in which two surgical disciplines sequentially perform robotic procedures, at distant anatomical sites, are extremely rare [6]. We present the first case of robotic surgery on the oropharynx and lung at a single sitting.
CASE REPORT
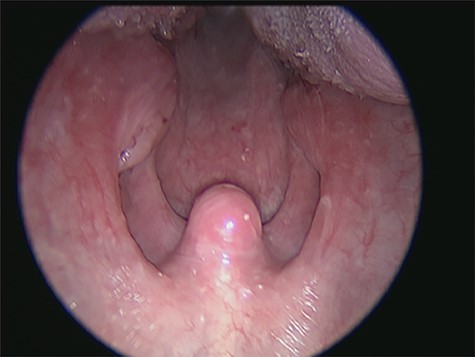
A 49-year-old male presented with a 7-week history of a neck lump. He had a 40-pack-year smoking history. His performance status was zero. Examination revealed a 3 cm × 2 cm fixed level II lymph node, an enlarged left tonsil (Fig. 1) and a bulky base of the tongue.
The patient underwent ultrasound-guided biopsy [7], revealing a metastatic lymph node: human papilloma virus (HPV)-positive and p16-positive squamous cell carcinoma (SCC). MRI neck showed soft tissue thickening within the left glossotonsillar sulcus, extending to the tongue base, and bulky, partially necrotic lymphadenopathy (Fig. 2). Panendoscopy and biopsy of the left tonsil showed non-keratinizing, HPV-associated SCC.
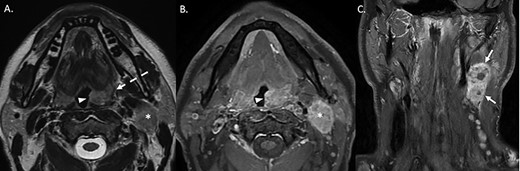
(A) T2-weighted axial sequence through the oropharynx, demonstrating asymmetric, exophytic enlargement of the left palatine tonsil (arrowhead). The signal within the middle constrictor is preserved (dashed arrow). An enlarged level II lymph nodal lesion is also noted (asterisk). (B) Axial post-gadolinium fat-suppressed sequence at the same anatomical level demonstrates heterogeneous enhancement of the enlarged let palatine tonsil (arrowhead). The ipsilateral level 2 nodal lesion is also noted (asterisk). (C) Coronal post-gadolinium fat-suppressed sequence demonstrates a conglomerate nodal mass at level 2–3 on the left with areas of central non-enhancement compatible with necrosis.
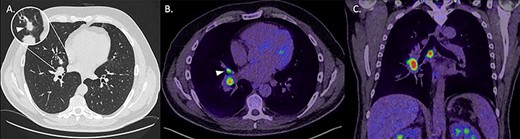
(A) Axial non-contrast CT thorax on lung windows demonstrating a 13-mm, spiculated perihilar lesion within the middle lobe of the right lung (magnified). (B) Axial fused image from a PET-CT demonstrating elevated uptake within the middle lobe lesion (arrowhead) as well as within enlarged ipsilateral hilar lymph nodes. (C) Coronal fused image from a PET-CT demonstrating increased uptake in abnormal right hilar and subcarinal lymph nodes.
CT thorax showed a 1.3 cm spiculated right middle lobe nodule, concerning for a primary lesion. Subsequent PET-CT showed intense uptake there and in the right hilum and a sub-carinal lymph node (Fig. 3). An endobronchial ultrasound bronchoscopy showed adenocarcinoma in station 11R and 7. Diagnoses of T2N1M0 left tonsil SCC (TNM 8 classification) and T2N2 (single station) M0 adenocarcinoma were made.
Primary chemoradiotherapy would be the common management strategy. However, a multidisciplinary discussion concluded that this would be too morbid [5]. Conventional surgery on two anatomical sites would also have entailed significant morbidity. A synchronous minimally invasive approach, followed by adjuvant treatment, was therefore recommended. A left neck dissection was undertaken, followed, a week later, by sequential robotic oropharyngeal and thoracic procedures.
The robotic procedures were undertaken with the DaVinci Xi system. The head and neck team performed a left lateral oropharyngectomy via TORS in 90 minutes. Video 1 demonstrates the key steps.
On completion of the TORS, a single-lumen airway was replaced with a double-lumen and a paravertebral block inserted, taking approximately 20 minutes. During this time, drapes on the robot were changed, scrub nurses replaced and thoracic robotic instruments prepared. The thoracic team then performed a robotic right middle and lower bilobectomy and full lymph node dissection in 5 hours. Video 2 demonstrates the key steps of this procedure.
The total procedure time was 7 hours, and the estimated blood loss was less than 300 mL. Histopathology confirmed complete excisions. The patient was extubated and transferred to the critical care unit (CCU). Nasogastric (NG) feed was commenced, but with quick progression to a soft diet, the NG tube was removed on post-operative Day 4. The patient was discharged from the CCU on post-operative Day 3 and home on Day 6, with a chest drain in situ for a persistent air leak. The drain was removed after 2 weeks. Radiotherapy commenced 3 weeks post-operatively.
Shortly after starting radiotherapy, the patient was re-admitted with a small bronchopleural fistula. This was closed using an intercostal muscle flap. Despite this complication, the patient was able to continue with, and complete, adjuvant therapy. Six months post-operatively, the patient is fully recovered with a performance status of one.
DISCUSSION
Undertaking two robotic procedures in a single sitting presented unique challenges to the anaesthetic team. The challenges of any robotic surgery, such as positioning and length of procedure, were magnified in this case [8]. Additionally, the TORS required a single-lumen airway, while the RATS required a larger double-lumen airway for one-lung ventilation. The decision was made to start with the TORS. This entailed the risk of potential subsequent difficulty inserting the required larger airway, due to bleeding and oedema. However, starting with the thoracic procedure would have risked dependent oedema from the patient lying on his side. The TORS necessitated awake nasal fibre-optic intubation because of the patient’s relatively large body habitus, tumour size, and to ensure that the endotracheal tube was clear of the operating field.
Consideration was also given to antisepsis, given that we started with a clean-contaminated transoral procedure, which was followed by a thoracic approach. Hence, drapes on the robot were changed, a new scrub team deployed, and a new set of robotic instruments readied for the thoracic procedure. The total procedure length was 7 hours; therefore, dependent oedema and its potential effect on extubation also had to be considered. There was a need for a thorough post-operative analgesia plan given the two-site surgery and the risks of poor cough and aspiration.
The precise dissection facilitated by robotic surgery helped to mitigate potential risks by minimizing bleeding and the chance of nerve injury. Joint surgery using conventional, open approaches would have been considered high risk and necessitated a significant time interval between procedures, with two lengthy inpatient stays. A robotic minimal-access approach allowed us to resect both primaries and undertake both lymphadenectomies in two sittings and two short stays.
Post-operatively, the patient experienced a prolonged air leak—a common complication post-bilobectomy due to the large dead space and the extensive hilar dissection [9]. Despite this, it was possible to discharge him 1 week post-operatively, and he was able to start radiotherapy within 3 weeks.
During radiotherapy, the combination of a chest infection and steroid treatment contributed to the development of a bronchopleural fistula—a well-known complication in extended resection. The patient’s quick recovery from minimal-access surgery allowed us to surgically address the bronchopleural fistula immediately. This primary repair had a good outcome, which allowed the patient to continue chemoradiotherapy. The combined, sequential robotic approach therefore expedited not only the patient’s initial surgical treatment but also adjuvant therapy and the management of complications.
ACKNOWLEDGEMENTS
We would like to thank Dr Philip Touska, Consultant Head and Neck Radiologist, Guy’s and St Thomas’ NHS Foundation Trust, London, UK, who provided annotated images of cervical and thoracic disease; Miss Aina Brunet, Head and Neck Fellow, Guy’s and St Thomas’ NHS Foundation Trust, London, UK, who assisted in the TORS procedure; Mr Igor Saftic, Thoracic Surgery Fellow, GSTT, who assisted in the thoracic procedure; Liza R D Mills, Surgical Care Practitioner; and theatre staff Ricardo Vendicil, Nicole Palec and Rachael Parker.



