-
PDF
- Split View
-
Views
-
Cite
Cite
Christopher Maguire, Pirathaban Sivabalan, Shaurya Jhamb, Pranavan Palamuthusingam, Hepatic tuberculosis masquerading as cholangiocarcinoma: an unusual differential for a liver mass, Journal of Surgical Case Reports, Volume 2020, Issue 8, August 2020, rjaa247, https://doi.org/10.1093/jscr/rjaa247
Close - Share Icon Share
Abstract
A 54-year-old woman presented with an incidentally identified asymptomatic liver lesion with imaging characteristics suspicious for malignancy. She underwent a left hemihepatectomy for presumed cholangiocarcinoma. Histopathology revealed granulomas with microbiological investigations later revealing a diagnosis of isolated hepatic tuberculosis. There were no pulmonary or other disease sites identified. The patient has been medically managed for primary hepatic tuberculosis and remains well postoperatively. This case identifies a rare differential for a liver mass that needs to be considered in the clinicians’ workup.
INTRODUCTION
By international standards, the Australian annual incidence of tuberculosis is low (~5–6 cases per 100 000 population) [1]. Therefore, when it presents atypically, clinical suspicion is often low, and the diagnosis can easily be missed. We present a case of a 54-year-old female with an incidental hepatic lesion resected for concerns of malignancy; however, it was found to be local hepatic tuberculosis.
CASE REPORT
A 54-year-old female, of Philippines descent, presented to our department following the incidental discovery of a 23 × 20 mm ill-defined mass within segment II/III of the liver during ultrasound workup for mildly deranged liver function tests. She had no symptoms from the lesion, and she reported no significant past medical history. A pre- and post-contrast multiphase helical computed tomography identified a 26 × 25 mm ill-defined region of hypodensity, with a small focus of central calcification, within segments II and III of the liver (Fig. 1). The lesion was causing biliary obstruction indicated by dilatation of the intrahepatic biliary ducts within the entire left lobe of the liver and appeared to be in continuity with the left hepatic duct. Magnetic resonance imaging of the liver identified an irregular enhancing mass within segment IV that had a central area of non-enhancing low signal intensity (Fig. 2). As a part of the patient’s workup for presumed malignancy, an upper and lower endoscopy, bilateral mammogram and ultrasound assessment of the breasts were all found to be normal. A biopsy was not able to be obtained due to the proximity of the lesion to the porta hepatis.
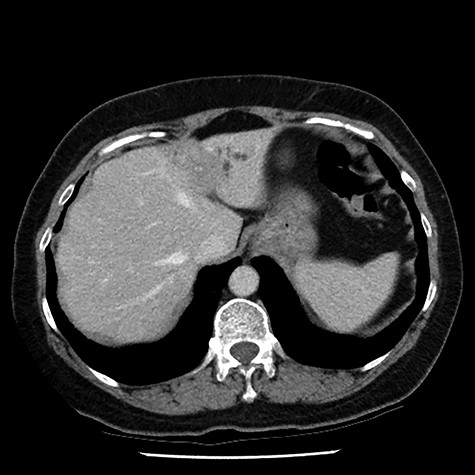
post-contrast multiphase helical computed tomography identified a 26 × 25 mm ill-defined region of hypodensity, with a small focus of central calcification, within segments II and III of the liver
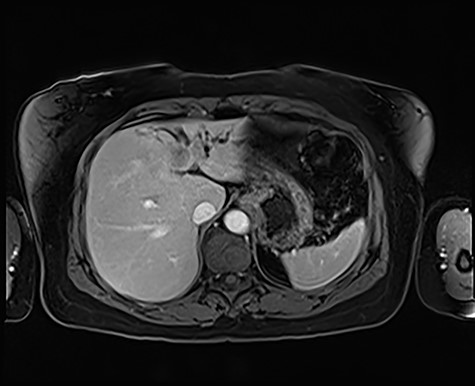
magnetic resonance imaging, T2-weighted image demonstrating an irregular, enhancing mass within segment IV that has a central area of non-enhancing low signal intensity
Based on these findings, the decision was made to proceed to open resection. An open left hemihepatectomy was performed with complete removal of the mass. Histopathology revealed necrotizing granulomatous inflammation (Fig. 3). Mycobacteriology assessment revealed no acid-fast bacilli. However, mycobacterial nucleic acid amplification testing
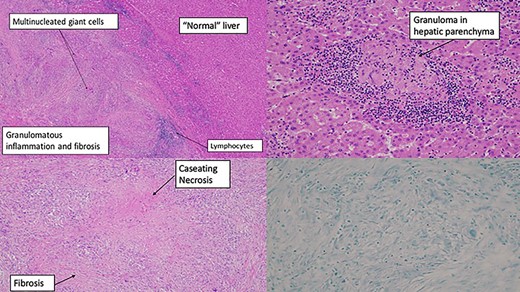
(A) resected liver specimen—routine formalin-fixed tissue stained with haematoxylin and eosin. Granulomas and fibrosis with demarcation with adjacent normalish liver parenchyma. (B) Resected liver specimen—routine formalin-fixed tissue stained with haematoxylin and eosin showing a necrotizing granuloma surrounded by lymphocytes within the liver parenchyma. (C) Biliary duct—routine formalin-fixed tissue stained with haematoxylin and eosin. Granulomas centred around an intrahepatic bile duct, replacing some of the epithelium. (D) Bottom right—Ziehl–Neelsen stain (negative for acid-fast bacilli)
(GeneXpert Assay {IS6110}) identified deoxyribonucleic acid for Mycobacterium tuberculosis, and mycobacterial culture of the operative specimen cultured the same, with a sensitivity profile suggestive of drug-susceptible tuberculosis. The patient had an uncomplicated post-operative course and is successfully undergoing medical management for hepatic tuberculosis.
DISCUSSION
According to the Levine classification, our case likely represents primary hepatic tuberculosis [2]. Primary tuberculosis is rare and represents ~1% of all instances of the disease [3]. Where clinical features are present, the most common are right upper quadrant pain, anorexia, weight loss and fever [4]. In our case none of these were evident. Even when clinical symptoms and signs do exist, diagnostic difficulty has been well documented in the literature [5, 6]. This is due to the similarity in clinical presentation and imaging characteristics of primary hepatic tuberculosis and hepatobiliary malignancy [7]. In this instance, given the concerning imaging features of the lesion and our inability to obtain a pre-operative tissue biopsy, our approach was to treat the patient as if it were a malignancy until proven otherwise. This raises the question of what, if any, diagnostic tools could help differentiate these cases in the future. In our case the patient reported no exposure history of tuberculosis, had no clinical features of the disease and presented based on an incidental imaging finding. In retrospect, the patient’s ethnic background was the only suspicious aspect of her case. The rate of tuberculosis in overseas-born members of the Australian population in the most recent reported data was 17 times higher than the rate in the Australian-born population. Moreover, the Philippines was one of the five most frequently reported countries of birth for tuberculosis cases in Australia [1]. Notwithstanding those facts, even had there been clinical suspicion, the diagnosis remains challenging. The sensitivity of acid-fast bacilli staining is low, especially for extra-pulmonary tuberculosis cases [8]. Percutaneous biopsy is reliable but, as was the case in our patient, may not be feasible and also presents the small but serious potential for seeding of malignancy along the diagnostic tract. Laparoscopically assisted liver biopsy is therefore the safest and most reliable means of differentiating cases; however, it also potentially necessitates two operations. Our recommendation would be that in patients in which there is a high degree of clinical suspicion and uncertainty exists, a laparoscopically assisted liver biopsy, if feasible, should be considered—with specimens analysed for histology, acid-fast bacilli, mycobacterial cultures and most importantly tuberculosis polymerase chain reaction. These are reasonable workup modalities to ensure hepatic tuberculosis is considered prior to aggressive surgical resection of the lesion. If these investigations are negative for tuberculosis, then we would recommend resection with specimens sent for histopathology and mycobacterial assays to further delineate the diagnosis.
Conflict of interest statement
None declared.



