-
PDF
- Split View
-
Views
-
Cite
Cite
Masanori Kanemura, Atsushi Yoshida, Akihiko Toji, Sousuke Hashida, Yumi Murayama, Emi Iwai, A case of pyometra with a colouterine fistula due to rectal cancer presenting as acute abdomen, Journal of Surgical Case Reports, Volume 2020, Issue 8, August 2020, rjaa237, https://doi.org/10.1093/jscr/rjaa237
Close - Share Icon Share
Abstract
Pyometra usually develops in elderly women, and it can be caused by various etiologies. We describe a rare case of pyometra with a colouterine fistula due to rectal cancer presenting as acute abdomen. A 67-year-old woman with purulent vaginal discharge and abdominal distension was referred to our hospital for suspected pyometra. Because the vaginal echogram showed pyometra at her initial medical examination, drainage was performed. Her symptoms subsequently disappeared temporarily, but 4 months later, she developed acute abdomen. The computed tomography scan showed a pelvic mass with expansion of the intestine. The patient underwent en bloc resection of the mass. Histopathologic analysis of the tumor showed rectal cancer with invasion of the uterus and ileum, and a colouterine fistula. Although pyometra due to a colouterine fistula is a very rare condition, the incidence of associated malignancy is considerable. Physicians should be aware of this potential presentation of colorectal cancer.
INTRODUCTION
Pyometra is the accumulation of purulent contents in the uterine cavity [1], which may or may not be associated with malignancy. It usually develops in elderly women and has an incidence of 0.1–0.5% [2]. The most common presenting symptom is postmenopausal bleeding, followed by vaginal discharge. Pyometra can be treated with drainage and antibiotics [3]. Pyometra may rarely cause sloughing of the uterine wall and spilling of pus into the abdominal cavity, leading to symptoms of acute abdomen. We herein describe a rare case of pyometra with a colouterine fistula due to rectal cancer presenting as acute abdomen and provide a literature review.
CASE PRESENTATION
A 67-year-old postmenopausal woman, gravida 0, presented with purulent discharge and abdominal distension. Her past medical, surgical, gynecological and family histories were all unremarkable. The vaginal examination showed a foul smelling, green vaginal discharge and no tenderness of the uterus. Vaginal swab cultures grew Escherichia coli. The endometrial Papanicolaou test was negative. Laboratory results, including the blood count, differential, liver function and renal function, were within the normal range. There was no fever, weight loss or palpable lymphadenopathy and organomegaly. The transvaginal ultrasound image showed the presence of hypoechoic fluid in the uterine cavity, compatible with a diagnosis of pyometra (Fig. 1). Drainage of the purulent contents by uterine Foley catheter insertion was performed. The culture of the pus grew Klebsiella pneumoniae and E. coli. After draining the fluid, her symptoms disappeared temporarily. However, 3 months later, she was admitted to our hospital with abdominal pain that gradually worsened. On physical examination, her abdomen was very tender and showed diffuse peritoneal signs. Her vital signs were stable, but laboratory studies detected a mild increase in the levels of leukocytes (9510/μl) and C-reactive protein (1.24 mg/dl). The carcinoembryonic antigen (CEA) level was significantly increased (10.2 U/ml), and the cancer antigen-125 level was slightly increased at 102.7 U/ml. The magnetic resonance imaging scan demonstrated a pelvic mass involving
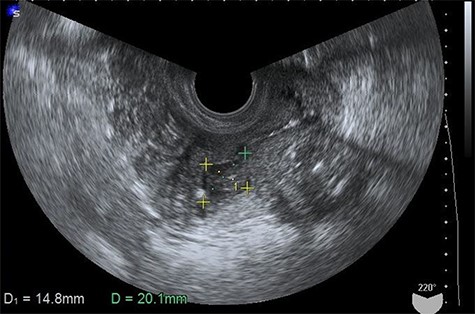
Transvaginal ultrasonogram showing the presence of hypoechoic fluid in the uterine cavity.
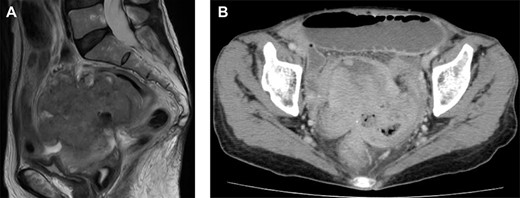
Magnetic resonance imaging and computed tomography (CT) findings preoperatively. (A) Sagittal T2-weighted MRI scan demonstrating a pelvic mass involving the uterus and rectum. (B) CT scan showing expansion of the intestines and the absence of free intraperitoneal air.
the uterus and rectum (Fig. 2A). The computed tomography scan showed expansion of the intestines and no evidence of free intraperitoneal air (Fig. 2B). As she had a history of bloody stool and the CEA level was increased, we performed colonoscopy, which showed a malignant tumor of the rectum (Fig. 3). The protruding tumor was located 7 cm from the anus. Exploratory laparotomy showed a 90-mm pelvic mass involving the uterus, ileum and rectum. Therefore, we performed an en bloc resection of the mass, including total hysterectomy, bilateral salpingo-oophorectomy, partial resection of the ileum and the Hartmann operation. Macroscopically, the resected pelvic mass invaded the uterus, intestine and rectum, and a colouterine fistula was identified (Fig. 4). The main portion of the tumor was located in the rectum, and it grossly appeared that tumor invasion occurred from the rectum to the uterus and ileum. Microscopic examination of the pelvic mass showed complicated glandular structures in a desmoplastic stroma. The cells forming the lumen were primarily columnar epithelium, consistency of the small glandular cavity was high and severe dyskaryotic cells were multilayered. The nuclei were enlarged and irregularly shaped, contained coarse chromatin and showed atypia. Immunohistochemical staining was performed. Cytokeratin (CK)20 (Dako), NCL-Villin (Novocastra) and CEA (Dako) were positive, and CK7 (Dako) was negative. The final diagnosis was moderately differentiated tubular adenocarcinoma of the rectum, stage IIC, pT4b N0 M0. The patient’s postoperative course was uneventful. The serum level of CEA returned within normal range 1 month postoperatively. Adjuvant chemotherapy (TS-1) was administered for 6 months postoperatively. The patient has been followed up with for >12 months without any signs of recurrence.
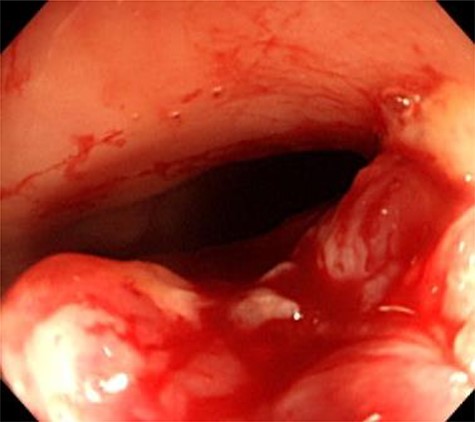
Colonoscopy findings. Colonoscopy showed a malignant tumor of the rectum. The tumor was localized, and invasion outside the colonic wall was suspected.
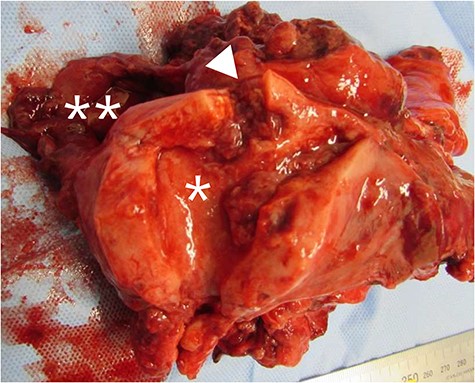
Macroscopic findings of the uterus. The uterus (*), intestine and rectum (**) formed a solid mass, and a colouterine fistula (arrowhead) was present.
DISCUSSION
Pyometra occurs primarily in elderly postmenopausal women due to conditions that interfere with the natural drainage of the uterus, including cervical stenosis and various other diseases, such as malignant tumors [4]. The most common presenting symptom is postmenopausal bleeding (59.2%), followed by vaginal discharge (40.8%), fever (6.6%) and abdominal pain (5.3%) [3]. More than 50% of patients with unruptured pyometra are asymptomatic [5]; most patients with perforation associated with pyometra have abdominal pain. Spontaneous perforation of pyometra is a very rare condition, with an incidence of 0.01–0.05% in gynecological patients [6]. According to a literature review of spontaneous perforation of pyometra, the total number of patients with a malignant tumor was 18 (34%) among 53 patients with a diagnosis confirmed by histological analysis. Among patients diagnosed with a malignant tumor, colorectal cancer occurred in five patients (28%) [4].
Once pyometra is ruptured, morbidity and mortality increase, clinical symptoms become much more severe in intensity, and acute abdomen occurs, which most often requires prompt emergency surgical intervention [2]. The mortality from spontaneously perforated pyometra is reportedly 15.2%, and in immunocompromised patients, the mortality rate is increased [7].
A colouterine fistula is an extremely rare condition, because the thick muscle of the uterus protects from invasion by benign and malignant disease. Several reports have been published about colouterine fistulas caused by diverticulitis of the sigmoid colon [8]. There are few reports on malignancy associated with a colouterine fistula [9, 10]. Unfortunately, our patient was diagnosed as having colorectal cancer invading the uterine body. The fistula developed between the rectum and uterus, leading to perforation of the uterine cavity. As a result, pus collected in the uterine cavity, resulting in pyometra.
Since there are few reports on a malignant colouterine fistula, its treatment has not been established. Halevy et al. performed en bloc resection in two patients with a malignant colouterine fistula, and they reported that this method offers better results [10]. In our patient, surgical resection was performed. Adjuvant chemotherapy was performed, and the patient has been free of recurrence for 12 months. As there are few similar reported cases in the literature, further study is necessary to determine the most appropriate treatment of this complication of colorectal cancer.
The diagnosis of pyometra due to a malignant colouterine fistula is difficult to make preoperatively. Gynecologists should keep in mind the possibility of a malignant colouterine fistula in patients with pyometra.
Conflict of interest statement
The authors have declared that no conflicting interests exist.



