-
PDF
- Split View
-
Views
-
Cite
Cite
Mohsen Ezzy, Thomas Kraus, Stefan Berkhoff, Oesophageal stenosis caused by giant multilevel anterior cervical osteophytosis, Journal of Surgical Case Reports, Volume 2020, Issue 8, August 2020, rjaa166, https://doi.org/10.1093/jscr/rjaa166
Close - Share Icon Share
Abstract
Dysphagia secondary to osteoarticular disorders is a rare entity. In this report, we present the case of a 76-year-old female patient with progressive dysphagia and recurrent aspiration pneumonia caused by large anterior cervical osteophytes. Osteophytectomy was performed without spinal fusion. The patient reported significant improvement post-operatively, and no recurrence was detected at the 1-year follow-up. Cervical osteophytosis should be suspected as a cause of dysphagia, especially in elderly patients with degenerative osteoarthritic disease when other causes have been excluded.
INTRODUCTION
Anterior cervical osteophytes (ACOs) are a common finding in degenerative spinal conditions, especially in elderly populations. There are multiple aetiologies for the pathogenesis of ACOs. The majority of cervical osteophytes occur secondary to degenerative diseases, such as cervical spondylosis. Other causes include diffuse idiopathic skeletal hyperostosis (DISH), ankylosing spondylitis, heterotopic ossification after cervical disc arthroplasty and prior neck trauma [1]. In the majority of cases, ACOs are asymptomatic. However, large ACOs can cause dysphonia, dyspnoea, dysphagia and pain [2]. Such symptoms are correlated with the size and location of the hypertrophic spurs. Dysphagia is a rare presentation of symptomatic ACOs. Here, we present the case of a 76-year-old female presenting with a large anterior osteophyte causing severe dysphagia whose symptoms resolved following surgical resection.
CASE PRESENTATION
A 76-year-old female patient without any known chronic medical illnesses was referred to our department with progressive dysphagia and recurrent aspiration pneumonia. The patient had lost 10 kg over a period of 15 months. She had experienced swallowing difficulty for the last 2 years. She denied a history of dyspnoea or dysphonia. She complained of frequent aspiration, especially when ingesting solid or semisolid food. She could tolerate a diet of only purees and liquids.
Her past history included right knee joint arthroplasty. There were no neurological manifestations, and there was no history of neck pain or trauma. The findings on physical examination were unremarkable. The routine blood test results were within the normal range. Oesophagoscopy revealed luminal stenosis by external compression on the posterior hypopharynx/oesophageal wall with no tumour or diverticula. Lateral neck X-ray and computed tomography (CT) examinations showed a giant anterior multilevel osteophytic formation spanning C4/5/6 and compressing the oesophagus, with no ossification of the anterior longitudinal ligament (Fig. 1A). A gastrografin swallow showed that osteophytes were severely protruding and impinging on the oesophagus, with partial obstruction (Fig. 1B).
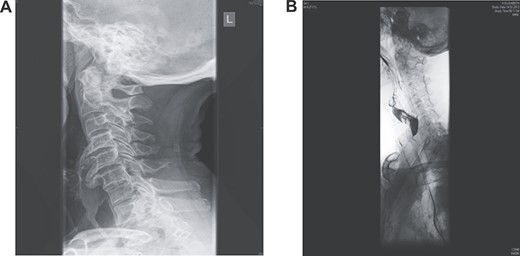
(A) Lateral X-ray reveals giant multilevel osteophytes at C4/5/6 compressing the oesophagus; (B) a gastrografin swallow showed that osteophytes were severely protruding impinging on the oesophagus with partial obstruction.
The patient underwent an anterior cervical osteophytectomy through an anterolateral approach (Fig. 2). Because of the advanced age and stable cervical vertebrae, no fusion or osteosynthesis was performed. No post-operative complications were encountered. Post-operative controlled X-ray examination revealed adequate resection of osteophytes (Fig. 3). Oral intake gradually advanced as tolerated. The patient was discharged on the third post-operative day without any neurological deficits. No evidence of recurrence was detected on lateral cervical X-ray examination, and the patient was free of symptoms at the 1-year follow-up.


DISCUSSION
Cervical osteophytes are bone spurs that can involve any vertebra in the cervical spine.
They are rounded and scalloped in shape. Spinal osteophytes are considered a normal sign of ageing and typically occur when ligaments and tendons around the cervical spine are damaged or inflamed. This process usually occurs with wear and tear over time [3].
Many people with cervical osteophytes are asymptomatic. However, large cervical osteophytes may produce a wide range of symptoms secondary to the encroachment of nearby structures, causing neck pain and stiffness, cervicogenic headache and myelopathy. In advanced cases, the patient may experience dysphagia, dyspnoea, dysphonia and aspiration [4].
Giant cervical osteophytes leading to dysphagia are rare but must be considered in the elderly in the differential diagnosis of dysphagia.
A total of 10.6% of patients presenting with dysphagia have cervical osteophytes [5]. In contrast, 17% of patients with cervical osteophytosis develop dysphagia [6].
Dysphagia associated with ACOs is mainly caused by secondary mechanical compression and displacement of surrounding structures [7]. Concomitant inflammation and fibrosis may exacerbate the situation. Dysphagia is often seen with the ingestion of solid foods and is usually progressive over time.
DISH, known as Forestier’s disease, is one of the common causes of anterior cervical hyperosteophytosis. It is estimated that 3% of individuals over the age of 40 have DISH, and 0.1–6% of those will develop dysphagia [8]. Major diagnostic criteria for DISH include ossification along the anterolateral aspect of at least four contiguous vertebral bodies, relative preservation of the intervertebral disc height and the absence of apophyseal joint ankylosis or sacroiliac joint sclerosis [9]. Our case did not meet the DISH criteria.
In suspected cases, simple lateral neck radiography must be applied as an initial diagnostic tool. Oesophagoscopy and barium swallow are important to evaluate the degree of stenosis and rule out other causes of dysphagia. A CT scan is required to confirm the diagnosis and delineate the anatomy. Magnetic resonance imaging is also helpful, especially if there are neurological manifestations.
The management of patients with cervical osteophytes has to be individualized, depending on symptom severity. Conservative treatment is recommended initially. Surgical treatment should be considered in refractory cases with severe symptoms.
CONCLUSION
Cervicogenic dysphagia caused by cervical osteophytes is a rare presentation that must be considered, especially in elderly patients with osteoarthritic degenerative disease. Routine lateral neck X-ray examination is a simple, affordable and valuable initial diagnostic tool for cervical osteophytosis. Surgery is indicated when the symptoms are severe and progressive. Periodic follow-up is important to monitor for signs of recurrence.
AUTHORS CONTRIBUTIONS
ME contributed to the literature review, data collection, writing, subsequent revision and submission of the report. SB revised the paper, cared for the patient and was part of the team that performed the operation. TK supervised the project and contributed to revision of the report. All authors approved the content of the final manuscript.
CONFLICTS OF INTEREST STATEMENT
None declared.
FUNDING
None.
ETHICS APPROVAL
Not applicable. This is a case report based on the clinical notes of an individual patient, and written consent for publication has been obtained from the patient.
CONSENT
Written informed consent was obtained from the patient for the publication of this case report and accompanying images.



