-
PDF
- Split View
-
Views
-
Cite
Cite
K V Chalam, Moises Enghelberg, Ravi K Murthy, Allergic fungal sinusitis masquerading as cavernous sinus thrombosis, Journal of Surgical Case Reports, Volume 2020, Issue 8, August 2020, rjaa233, https://doi.org/10.1093/jscr/rjaa233
Close - Share Icon Share
Abstract
Allergic fungal sinusitis (AFS), a noninvasive form of fungal sinusitis, is rarely seen in immunocompetent patients. Involvement of sphenoid sinus can result in proptosis and loss of vision. We report AFS masquerading as posterior cavernous sinus syndrome. A 59-year-old African-American man presented with right complete ptosis with ophthalmoplegia. After an initial work-up and imaging studies, patient underwent endonasal sphenoid surgery, which revealed characteristic ‘allergic fungal mucin’. Cavernous sinus syndrome is a rare presenting clinical feature of allergic fungal sinusitis. Ophthalmologists should be aware of this rare presentation of relatively common otorhinological disease for timely referral and appropriate management.
INTRODUCTION
Allergic fungal sinusitis (AFS), a noninvasive form of fungal rhinosinusitis, accounts for 6–9% of all rhinosinusitis that require surgery [1]. Common presenting features in patients with AFS include rhinosinusitis with nasal polyps, atopy and elevated total serum immunoglobulin E (IgE) [1, 2].
Involvement of sphenoid sinus with bony erosion and extension into orbit leads to ocular symptoms including proptosis, diplopia and decreased vision [3]. Though orbital involvement with vision loss in AFS is known, isolated involvement of cavernous sinus is rare.
In this report, we describe a patient with AFS who presented with clinical features of posterior cavernous sinus syndrome.
CASE SUMMARY
A 59-year-old African-American male, Jamaican in origin and a farmer by profession, was evaluated in the emergency room with sub-acute onset of headache and ptosis of right upper eyelid of 3 weeks duration. He initially presented to his primary care physician with continuous headaches in the frontal area for which he was prescribed Bactrim™ (AR Scientific Inc., Philadelphia, PA).
His symptoms continued to worsen with complete ptosis and he was admitted for further evaluation. He denied any pain, redness and visual disturbance in both eyes. His past medical history was significant for systemic hypertension, which was adequately controlled. Review of systems was negative for epistaxis, fever, allergies and asthma. On examination, his visual acuity was 20/20 and intraocular pressures were 15 mm Hg in both eyes. Color plates were full on Ishihara color plates, and there was no proptosis on Hertel’s exophthalmometer. Pupils were 2 and 3.5 mm in right and left eye, respectively, with no apparent difference in anisocoria in darkness and light. There was complete ptosis of right upper eyelid, and right eye was completely frozen in primary gaze with full extraocular movements in left eye (Fig. 1 A and B). Corneal sensation was reduced on the right side along with sensation in the distribution of V1 facial area. Anterior segment and fundus examinations were unremarkable in both eyes. Rest of neurological examination was normal.

Clinical photograph of the patient’s upper face revealed a complete ptosis of right upper eyelid. Elevation of right upper eyelid and evaluation of extraocular movements revealed absence of right eye movement in dextroversion, levoversion, sursumversion and deorsumversion.
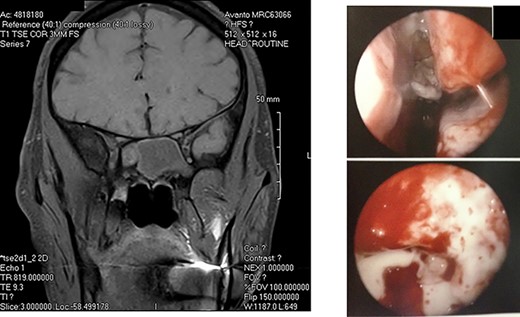
A: Magnetic resonance imaging (coronal view) reveals an expansile sphenoid sinus mass with fluid characteristics with extension into the cavernous sinus on the right. B: Intra-operative view through an endoscope reveals mucopurulent material from right sphenoid ostium. Sphenoid sinus reveals clumps of extramucosal ‘peanut buttery’ visco-elastic material (allergic mucin).
A diagnosis of right posterior cavernous sinus syndrome was made, and patient was subjected to imaging. CT scan revealed complete opacification of sphenoid sinus with bony erosion. MRI of brain revealed an expansile sphenoid sinus mass (with fluid characteristics on restricted diffusion) indicative of a pyo-mucocele (Fig. 2A). Complete blood counts were within normal limits and erythrocyte sedimentation rate was 95 mm/hour. Immunological work-up including serum anti-nuclear antibody, anti-cytoplasmic antibody and HIV were negative. Blood cultures were negative for bacteremia and fungemia. Patient was started on intravenous vancomycin, fluconazole and Decadron (Merck & Co., Inc., Whitehouse Station, NJ) was added after 48 hours. Five days after initiating treatment, no response was noted.
He was taken to the operating room, and an endoscopic exploration of sphenoid sinus was performed through sphenoethmoid recess. There was mucopurulent material drained through sphenoid ostium, and clumps of extramucosal ‘peanut buttery’ visco-elastic material (allergic mucin) were found in sphenoid sinus intra-operatively (Fig. 2B). One month post-operatively, patient’s visual acuity was 20/20, and extraocular movements revealed a minimal right abduction deficit.
DISCUSSION
In contrast to invasive fungal infections that are seen in immunocompromised patients, AFS occurs in immunocompetent patients. Common fungi implicated are Bipolaris, Curvularia, Alternaria, Fusarium and, rarely, Aspergillus [1, 2]. The exact pathogenesis of allergic fungal sinusitis is unknown but is believed to be an allergic reaction to the fungal elements and consists of a sinus-obstructing inspissates of a characteristic extramucosal ‘peanut buttery’ visco-elastic eosinophil-rich material called ‘allergic mucin’ that contains sparse numbers of fungal hyphae [2].
Diagnosis of AFS is based on history of type I hypersensitivity, presence of nasal polyposis, characteristic CT and MRI findings, presence of ‘allergic fungal mucin’ intra-operatively and staining for fungal hyphae on histopathology [4]. MRI findings (T1 central hypointensity and T2 central signal void) when combined with CT is highly specific [1]. However, histopathology can be inconclusive as yield is variable [5]. Diagnosis in our patient was based on the characteristic imaging and intra-operative findings.
Treatment of AFS is mainly surgical, aimed at debulking the sinuses and establishing drainage complemented by immunosuppression therapy in the form of oral or inhalational corticosteroids. Antifungal treatment has no role [1, 2].
In conclusion, cavernous sinus syndrome is a rare presenting clinical feature of allergic fungal sinusitis [6]. Ophthalmologists should be aware of this rare presentation of relatively common otorhinological disease for timely referral and management.
Conflict of Interest STATEMENT
None declared.
Funding
None.



