-
PDF
- Split View
-
Views
-
Cite
Cite
Hatem Adel Sembawa, Primary mesenteric gastrointestinal stromal tumor presented with acute small bowel obstruction, Journal of Surgical Case Reports, Volume 2020, Issue 8, August 2020, rjaa225, https://doi.org/10.1093/jscr/rjaa225
Close - Share Icon Share
Abstract
Primary mesenteric gastrointestinal stromal tumors may give rise to abdominal emergencies like bowel obstruction and should be considered in the differential diagnosis to reduce morbidity and mortality. The present study presents an unusual case of primary mesenteric gastrointestinal stromal tumor presenting with small bowel obstruction. A 44-year-old healthy male presented with abdominal pain for 2 days. Detailed examination revealed presence of a 4 × 4 cm mass in the small bowel mesentery with multiple small bowel loops adherent to it, together with their mesentery. The patient was diagnosed with primary gastrointestinal stromal tumor of the small bowel mesentery. He had an uneventful postoperative course and was discharged on the second postoperative day in a good condition. The case analysis showed that the diagnosis of gastrointestinal stromal tumor is likely with the emergence of CD117, despite of its occurrence at rare sites and it is a vague clinical picture.
INTRODUCTION
Primary mesenteric gastrointestinal stromal tumors are rare tumors, which present with vague clinical features. They are often clinically silent, until they reach a considerable size. Therefore, they are usually discovered incidentally and often at a late stage. They may give rise to abdominal emergencies like bowel obstruction and should be considered in the differential diagnosis to reduce morbidity and mortality. They are a rare cause of bowel obstruction but can be associated with significant morbidity.
Gastrointestinal stromal tumors constitute 85% of all mesenchymal neoplasms of the gastrointestinal tract [1]. They arise from the interstitial cells of Cajal, which are CD-117 positive spindle cells with minimal neural or myogenic phenotype [2]. These cells are pluripotential mesenchymal stem cells and the pacemaker cells of the gastrointestinal tract [3]. These tumors can occur anywhere in the gastrointestinal tract. Approximately, 70% of them originate from the stomach, with 20–30% occurring in the small intestine and mesentery [4, 5]. Their occurrence in the esophagus, appendix, colon and rectum is rare; however, there is occurrence of tumors on the omentum, mesentery or retroperitoneum found to be metastatic from gastric or intestinal primaries [5, 6]. They mainly occur in middle aged or older patients and are variable in size with an equal gender distribution. They are difficult to diagnose and are commonly diagnosed incidentally when they reach a significant size [1].
An abdominal mass with other signs of an indolent process is the usual presentation of primary mesenteric tumors [7]. They are often advanced at the time of definitive treatment. Their main presentations include; bleeding and obstruction caused by the growing tumor [8]. They are potentially malignant lesions that commonly metastasize to the liver and abdominal organs/peritoneum, but rarely to the skin, soft tissues and bones [8]. The present study has reported an unusual case of primary mesenteric gastrointestinal stromal tumor that presented with small bowel obstruction.
CASE REPORT
A previously healthy 44-year-old male was admitted to a health institution complaining of severe colicky abdominal pain for 2 days. It started suddenly and was continuous and diffuse; however, it was mainly in the right lower quadrant and was increasing in severity. He had never experienced similar pain in the past. The pain was associated with nausea, vomiting, hiccoughs, anorexia and bloating sensation. He had passed his last stool and flatus in the morning on the same day of admission.
On admission, he was alert and his vital signs, chest and cardiovascular examination were normal. The abdomen was distended, free of scars, and tender all over mainly in the right iliac fossa with guarding and a palpable mass with absence of bowel sounds. The hernia orifices were intact. The rectum was empty on digital rectal examination. His complete blood count and basic biochemical parameters were also normal. Contrast enhanced abdominal computed tomography scan showed an intra-abdominal mass associated with small bowel obstruction and a small amount of intra-peritoneal free fluid. Following a brief period of resuscitation, the patient was taken to the operating room for exploration. Upon examination, a 4 × 4 cm mass was detected in the small bowel mesentery with multiple small bowel loops adherent to it, together with their mesentery. There was no evidence of liver or peritoneal metastasis. Approximately, 1 m of small bowel had to be resected to completely excise the mesenteric mass with clear margins together with the adherent bowel and mesentery (Figs 1 and 2). Then, primary anastomosis was performed. The final pathology result was a grade 2 gastrointestinal stromal tumor with clear margins, mitotic index less than 2/10 high power field, maximum tumor size of 4 cm, and tumor cells were positive for CD117 (C-kit) and CD34. Hence, the final diagnosis was primary gastrointestinal stromal tumor of the small bowel mesentery. The patient had an uneventful postoperative course and was discharged on the second postoperative day in a good condition.
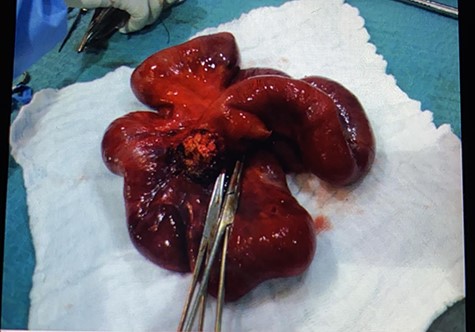
The resected segment of small bowel with part of the mesenteric tumor.
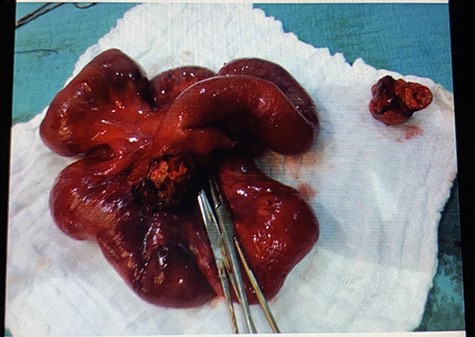
The resected segment of small bowel with part of the mesenteric tumor and a separate piece of it next to the resected segment.
DISCUSSION
Gastrointestinal stromal tumors have an uncertain biological behavior and arise in the gastrointestinal tract wall. They range from benign to malignant with a high capability to metastasize. Therefore, the outcome of patients suffering from these tumors is unpredictable and evaluation of their prognosis is limited [9]. The histological and clinical features of these tumors differ according to their primary site of origin [1]. They may cause both intraluminal bleeding and mass effects. Large tumors may lead to early satiety, vague abdominal pain or discomfort, and abdominal fullness. In rare cases, it presents with compression or obstruction of adjacent structures and spontaneous rupture into surrounding organs with possible intraluminal bleeding or into the peritoneum resulting in peritonitis with or without hemoperitoneum.
Plain X-rays or contrast studies may assist in the diagnosis in case of large masses or obstruction. Ultrasound is useful to identify cystic or solid components of the tumor. Computed tomography and magnetic resonance imaging is useful in detecting tumors larger than 2 cm [7]. Soft tissue tumors including these should be included in the differential diagnosis of any intra-abdominal mass with or without bowel obstruction. The decision for biopsy depends on the extent of the disease and the presence of a complication requiring urgent intervention, if the diagnosis of gastrointestinal stromal tumor is judged from its location (e.g. arising from the stomach or bowel wall). Therefore, confirmation of the tumor’s pathology is not necessary for localized, complicated tumors needing emergency surgery or potentially resectable appearing tumors for which neoadjuvant Imatinib therapy is not being considered.
Suryawanshi et al. [10] reported a case of gastrointestinal stromal tumor that presented as a mesenteric mass attached to the wall of ileum and presented as a case of sub-acute intestinal obstruction. Resection with negative margins (R0 resection) and without rupture of the pseudo-capsule or bleeding is the only recommended effective therapy for primary gastrointestinal stromal tumor in the absence of metastasis, if its technically feasible and risk of morbidity is acceptable with a long-term survival of up to 50% [1]. Prognosis depends on the size and completeness of surgical resection.



