-
PDF
- Split View
-
Views
-
Cite
Cite
Vladislav Borisov, Bram Stieltjes, Mark Wiese, Didier Lardinois, Reconstruction of the chest wall with a latissimus dorsi muscle flap after an infection of alloplastic material: a case report, Journal of Surgical Case Reports, Volume 2020, Issue 8, August 2020, rjaa213, https://doi.org/10.1093/jscr/rjaa213
Close - Share Icon Share
Abstract
Alloplastic material is often used for thoracic wall reconstruction following extended resection bringing the risk of infection, especially after chemotherapy and/or radiation. We present the case of a 66-year-old male with lung adenocarcinoma of the right lower lobe. After extended lobectomy, a partial resection of the sixth to eighth ribs followed by chest wall reconstruction with Mersilene mesh and osteosynthesis for sixth and seventh rib was performed. One month postoperatively, he developed pleural empyema. The alloplastic material was removed, extensive surgical debridement was performed and a latissimus dorsi muscle flap was used to cover the chest wall defect and fill out the remnant space supradiaphragmatically. Three years later, the patient has fully recovered with no local pain or relapse of the tumour. This case shows that rigid chest wall reconstruction with a soft autologous muscle flap is a valuable salvage option in case of infection, making alloplastic material highly risky.
INTRODUCTION
In its 2014 World Cancer Report, the World Health Organization (WHO) ranks lung cancer worldwide as the most common malignancy in men and the third most common in women. In ~5% of the operable cases, an invasion of the chest wall is found [1]. Depending on the size, location and whether a full thickness defect results from the extended resection, different approaches are considered optimal [2]. Alloplastic material is often used, bringing the risk of infection, especially after chemotherapy and/or radiation [3]. In this case report, we successfully demonstrate the use of a muscle flap as a strategy to reconstruct the rigid chest wall after infections.
CASE REPORT
A 66-year-old male ex-smoker (60 pack years) with chronic obstructive pulmonary disease (COPD) Gold II was successfully treated for pneumonia. During his treatment, a suspicious lesion was detected in the right lower lobe. A positron emission tomography–computed tomography (CT) scan showed a highly hypermetabolic tumour with suspicion of chest wall infiltration. A transbronchial biopsy confirmed an adenocarcinoma of the lung (Fig. 1). There was no evidence for distant or mediastinal lymph node metastasis. Pulmonary function showed an Forced expiratory volume in 1 second (FEV1) of 78.1%, vital capacity (VC) of 117% and a diffusion capacity of the lung for carbon monoxide by the single breath (DLCO cSB) of 70.8% of predicted value. Further examinations including spiroergometry and single-photon-emission computed tomography–CT confirmed functional operability up to bilobectomy. There were no major associated comorbidities.
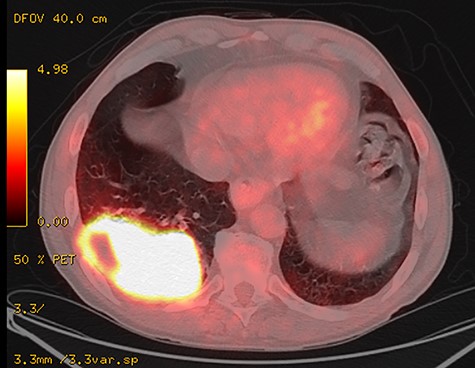
Positron emission tomography–CT scan of the primary tumour originating in the right inferior lobe and invading the adjacent thoracic wall.
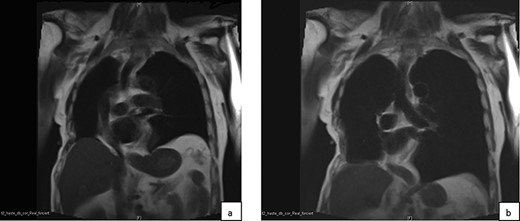
In dynamic magnetic resonance imaging examination of the thorax in coronary view in end-expiration (a) and end-inspiration (b) a paradox movement of the reconstructed area of the chest wall is observed.
During surgery, the posterolateral portion of the sixth to eighth ribs was resected en bloc with the right lower lobe and mediastinal lymph node dissection was performed. The chest wall was reconstructed with a Mersilene mesh and stability was achieved by the use of titanium plates (Stratos®, MedXpert, Germany) to overbridge the defect of the sixth and seventh rib. The definitive histological stage was pT3, pN0, cM0, R0, Union for International Cancer Control (UICC IIB).
One month after surgery, the patient developed a pleural empyema and resulting in rethoracotomy with removal of the Mersilene mesh and titanium plates combined with extended debridement. The defect of the chest wall, measuring ~5 × 5 cm, was sealed with vacuum-assisted closure (VAC) therapy and several debridements with change of the VAC system were performed for a total of 14 days. A latissimus dorsi muscle flap was prepared and mobilized in order not only to fill out the remnant supradiaphragmatic space, but also to close the chest wall defect, providing enough stability to the chest. Recovery was uneventful.
Three years after surgery, a dynamic magnetic resonance imaging examination and a lung function testing were performed in order to evaluate the long-term effects of the technique used on the stability of the chest wall and its functional relevance [4]. Paradoxical movement on the reconstructed side was observed there but there was no clinical or radiological evidence of relevant functional impairment (Figs 2 and 3). Pulmonary function showed an FEV1 of 60%, VC of 79% and a DLCO cSB of 70% of predicted value. The patient suffered from slight residual pain in the operated region with mild dysaesthesia. He describes his quality of life as very good.

The result 3 years after surgery in expiration (a) and deep inspiration (b) demonstrates a paradox movement locally.
DISCUSSION
Extended en block resection of the lung and chest wall is sometimes necessary to achieve complete oncological resection. In selected situations, especially after extended anterolateral resections, reconstruction of the chest wall is required to provide not only protection of the organs, but also to give enough stability for adequate respiratory function [2]. The general approach for the reconstruction of the chest wall consists of the use of alloplastic materials like meshes, sometimes reinforced with cement or titanium implants to provide enough stability [5]. Such procedures can be associated with a high incidence of infection, especially when chemotherapy and/or radiation were delivered prior to surgery. If an extended local paradoxical movement of the reconstructed chest wall would develop, it may lead to respiratory failure [6]. Generally, lesions <5 cm in size in any location may be reconstructed without the need of rigid prosthetic material [7]. In case of an infection, the use of alloplastic material is not recommended due to the formation of bacterial biofilm on the surface of the prosthesis that is usually unreachable for antibiotics and the immune system [8]. Thus, as in the case of our patient, an autologous muscle flap poses an excellent alternative material for the chest wall reconstruction. Several muscles flaps are available but the latissimus dorsi muscle flap is especially suitable for the coverage of wide resections [9]. A latissimus dorsi muscle flap can also be helpful in order to fill out residual space after extended pulmonary resection, providing well vascularised tissue and thus preventing recurrence of pleural empyema.
Usually, reinforcement of the reconstructed chest wall is not necessary when the defect is localized posterolaterally, like in our patient. In the majority of the cases, the paradoxical movement of the chest wall after reconstruction with muscle alone does not lead to respiratory insufficiency. Thus, in our clinical experience, the use of muscle flaps alone for reconstruction of the chest wall represents a good alternative to the classical approach with alloplastic materials, especially after induction therapy and infections. Although complete stability is often not reached, respiratory function and quality of life do not seem to be compromised.
CONFLICT OF INTEREST STATEMENT
No conflict of interest.
REFERENCES
- chemotherapy regimen
- debridement
- pleural empyema
- fracture fixation, internal
- reconstructive surgical procedures
- ribs
- surgical mesh
- surgical procedures, operative
- infections
- neoplasms
- pain, localized
- muscle transplantation
- lobectomy
- lung adenocarcinoma
- chest wall
- chest wall reconstruction
- latissimus dorsi flap
- infection risk
- rigid chest



