-
PDF
- Split View
-
Views
-
Cite
Cite
Preci Hamilton, Peyton Lawrence, Christian Valentin Eisenring, Metastatic epidural spinal cord compression, Journal of Surgical Case Reports, Volume 2020, Issue 8, August 2020, rjaa217, https://doi.org/10.1093/jscr/rjaa217
Close - Share Icon Share
Abstract
Up-to-date management for metastatic epidural spinal cord compression is based on appropriate scoring systems. In this case, separation surgery and stereotactic radiosurgery achieved an optimized outcome. A 75-year-old man had thoracic band-like pain, left lower limb weakness and difficulty ambulating for 6 weeks. Spinal images showed a T4 metastatic epidural spinal cord compression with a pathological fracture of T4 and T10 and L3 lytic lesions. There was no other neoplastic lesion. The metastasized T4 was decompressed by a posterolateral right costotransversectomy, vertebrectomy and insertion of an expandable titanium cage. The spinal sagittal alignment was restored with T1–T7 pedicle screw fixation. Post-operatively the pain and motor power improved significantly so that the patient was discharged home. Separation surgery and adjuvant stereotactic radiosurgery of the spine successfully improved tumor burden, pain control and overall prognosis.
INTRODUCTION
Metastatic disease to the spinal cord has a tendency to cause epidural compression and may manifest as myelopathy, radicular band-like pain or mechanical pain—a proxy for spinal column instability [1]. The best approach to individual cases including stage 4 disease requires careful multidisciplinary input with reference to scoring systems that take into account both patient and disease factors [2–5]. Improved technology has led to growing use of less invasive techniques such as percutaneous vertebroplasty, kyphoplasty, percutaneous pedicle screw instrumentation and less aggressive operative means such as separation surgery with adjuvant or stand-alone spine stereotactic radiosurgery (SSRS) [6, 7]. Separation surgery describes surgical decompression in order to provide a separation between the tumor and the spinal cord, thereby enabling the safe delivery of a cytotoxic radiation dose to the tumor while avoiding spinal cord toxicity and radiation-induced myelopathy [6].
Patchell solidified the role of surgery in metastatic epidural spinal cord compression (MESCC) having reported improved ability to walk (odds ratio 6.2 [95% CI: 2.0–19.8] P = 0.001) and maintaining ambulation for longer (median 122 days versus 13 days, P = 0.003) when surgery was offered compared to radiotherapy alone [8]. One area where surgery will never be replaced is the setting of established deformity with mechanical instability as this warrants structural support directed at restoring alignment, preserving mobility and optimizing pain control. We discuss a case of posterolateral decompression and stabilization for cancer of unknown primary (CUP) presenting as T4 MESCC with myelopathy as a result of thoracic pathological fractures.
CASE PRESENTATION
A 75-year-old man was referred to the spinal surgery unit at the hospital with left lower limb weakness and difficulty ambulating for 6 weeks. He had upper thoracic band-like pain, which was worse with walking [visual analogue scale (VAS) = 8/10], and he had been confined to bed for 2 days. He had no known neoplasm at the time, but he had a myocardial infarction 15 years previously. Clinical examination confirmed Medical Research Council scale for muscle power (MRC) grade 3/5 in his left lower limb, T6 sensory level and brisk lower limb reflexes.
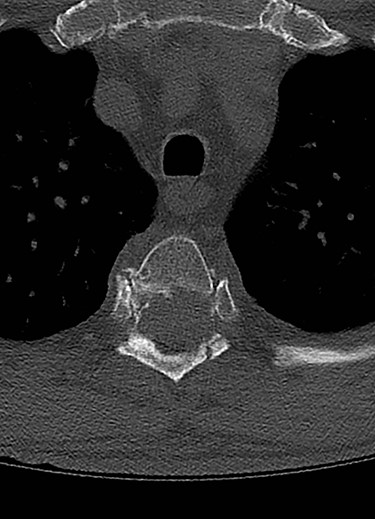
Spinal images are presented in Figs 1–6. Cross-sectional imaging revealed no other neoplastic lesion. He received dexamethasone 10 mg bolus then 4mg four times daily with appropriate proton pump inhibitor coverage. Due to no distinguishable major arterial feeder upon review of the imaging jointly with the neuroradiologist, pre-operative embolization was not attempted. The following morning, he underwent posterolateral right costotransversectomy, ligation of the ipsilateral T4 nerve root, T4 vertebrectomy and insertion of an expandable titanium cage with T1–T7 pedicle screw fixation (Figs 7 and 8). Post-operatively his pain improved to VAS 2/10 and motor power in his left lower limb improved to MRC grade 4/5. The patient was discharged home Day 10 post-admission with physiotherapy.
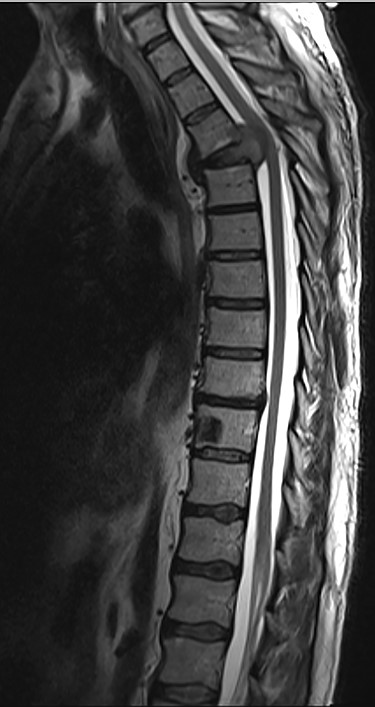
Sagittal T2-weighted magnetic resonance image (T2W MRI) with T4 metastatic epidural spinal cord compression (MESCC) and a synchronous T10 lytic lesion.
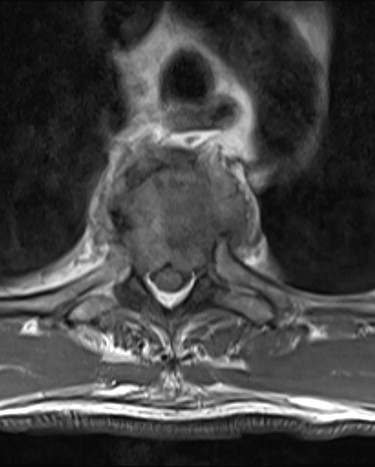

Sagottal T2W MRI showing synchronous lytic lesions in T10 & L3 vertebral bodies.

Sagittal computed tomography (CT) scan demonstrated multiple lytic lesions and pathological fracture of the T4 vertebra with almost complete collapse along with kyphotic deformity.

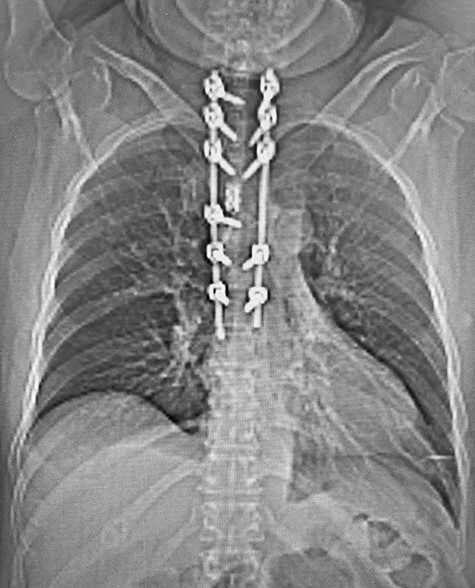
Post-operative CT with reconstructed anteroposterior view of the T1–T7 pedicle screw fixation and expandable titanium cage in situ.
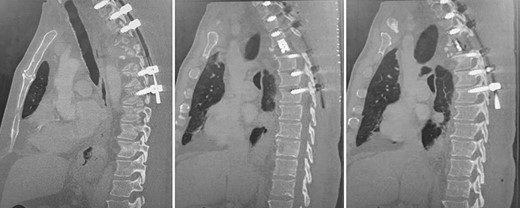
Post-operative, sagittal CT images of the T1–T7 pedicle screw fixation and expandable titanium cage in situ.
DISCUSSION
The patient presented with thoracic kyphosis and clinical evidence of mechanical pain. The radiological images showed evidence of three-column involvement of the T4 lytic lesion. Adjacent bilateral pedicle fracture of T5 offered no additional structural support and therefore this degree of deformity was not surprising. This spinal instability neoplastic score (SINS) [3] of 14/18 and grade 3 epidural spinal cord compression (ESCC) [2] were in support of surgical decompression and stabilization [2, 3]. A number of approaches were considered including anterior transcavitary, posterolateral extrapleural approaches and posterior decompression and instrumentation, with or without insertion of expandable titanium cage [1]. Laminectomy alone or with radiotherapy was not an option in this case as it would have offered very little decompression of this anteriorly compressing lesion as well as exacerbate the deformity by further sacrificing the posterior elements, thereby offering no contribution at structural stability.
The Tomita score considers the primary tumor growth potential as a guide for consideration for major surgery [5]. Yet another such scoring system is the Tokuhashi system, which considers similar parameters but takes into account the patient’s general performance status and neurological status [4]. The Tomita score of 4 and Tokuhashi score of 9 predicted a survival of 1–2 years and <6 month, respectively [4, 5].
The posterolateral approach—current evidence
Anterior decompression was not favored as a posterior approach was a less morbid alternative particularly at this level of the upper thoracic spine [1]. Furthermore, the posterolateral costotransversectomy offered adequate exposure of the T4 vertebra and allowed satisfactory anterior decompression [1]. Open pedicle screw placement was done, as the decompression and cage insertion would necessitate significant dissection albeit at one level.
The contemporary literature supports separation surgery for radiosensitive histology [9]. SSRS to the three spinal lesions identified would increase the likelihood of delivering a cytotoxic dose to the metastases with a reduced risk for collateral damage to organs at risk (OAR) especially the spinal cord [7]. In this case, however, vertebrectomy was necessary to achieve deformity correction by inserting the expandable cage in the anterior column.
In the index case, an expandable cage with anterior support was additionally put in place; therefore the implant failure rate tends to be smaller given this load sharing advantage.
Role of vertebroplasty/kyphoplasty
Percutaneous vertebroplasty with polymethyl methacrylate (PMMA) has been shown to safely improve pain associated with MESCC and disability [10]. In this case, however, there was no role for cement augmentation as there would be a significant risk of leakage into the spinal canal and intervertebral disc spaces with potential devastating pain and neurological deficits given the involvement of the T4 posterior vertebral body and endplates.
Surgical stabilization is irreplaceable in the management of MESCC with mechanical instability such as in this case. This patient warranted decompression of an anteriorly compressing lesion, and the posterolateral approach allowed all surgical goals: decompression, stabilization and deformity correction to be accomplished.
The individualized hybrid therapy with separation surgery and adjuvant SSRS successfully improved tumor burden, pain and overall prognosis.
ACKNOWLEDGEMENTS
We would like to thank Mr Antonino Russo for insightful management guidance and manuscript reviews. There was no previous presentation of this manuscript in a conference and no funding resources.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



