-
PDF
- Split View
-
Views
-
Cite
Cite
Manuela Pastoricchio, Andrea Dell’Antonio, Massimo Zecchin, Elisabetta Bianco, Annalisa Zucca, Alan Biloslavo, Marina Bortul, An uncommon case of inferior vena cava injury during atrial fibrillation ablation, Journal of Surgical Case Reports, Volume 2020, Issue 8, August 2020, rjaa201, https://doi.org/10.1093/jscr/rjaa201
Close - Share Icon Share
Abstract
A 64-year-old man underwent catheter ablation (CA) of atrial fibrillation with intracardiac echocardiography (ICE) assistance. As the probe was advanced toward the right atrium, sudden abdominal pain was felt by the patient with hypotension and tachycardia requiring fluids and vasopressors for hemodynamic stabilization. The inferior vena cava (IVC) was injured by the passing probe and open repair was then performed. To our knowledge, this is the first reported case of symptomatic IVC laceration by the probe used for ICE during CA.
INTRODUCTION
Catheter ablation (CA) has revolutionized the treatment of drug refractory atrial fibrillation (AF), employing radiofrequency or cryoenergy to cause scarring of abnormal electrical areas. Recent data from the European EurObservational Research Programme (EORP) Pilot registry show an overall complication rate of 7.7% with major complications occurring in 1.7%, mostly represented by vascular (pseudoaneurysms, arteriovenous fistulas, hematomas or bleeding) and cardiac complications (mainly pericarditis and cardiac perforation) and cardioembolic events (stroke/transient ischemic attack) [1]. The introduction of standard tools in AF ablation procedures, as intracardiac echocardiography (ICE), has reduced potentially life-threatening complications such as pericardial effusion and thrombus formation, due to real-time visualization of cardiac structures and continuous monitoring of catheter location within the heart during CA [2–4]. On the other hand, systemic anticoagulation regimens to prevent more serious complications (i.e. thromboembolism and stroke), in the background of multiple vascular accesses with moderate-to-large sheaths, trans-septal punctures and catheter manipulation, have increased risk for bleeding complications [5–8]. Although generally self-limited or managed conservatively, bleeding may rarely be encountered as a life-threatening situation requiring surgical intervention.
CASE REPORT
A 64-year-old man with a 3-year history of symptomatic drug refractory paroxysmal AF in multifactorial dilated cardiomyopathy (hypertensive, valvular and post radio-chemotherapy heart disease) was referred to our hospital for CA. Warfarin was stopped 3–4 days before the procedure and weight-adjusted doses of low molecular weight heparin (LMWH) were administered. Preprocedural echocardiography and enhanced computed tomography (CT) revealed no vascular anatomic anomalies. The procedure was performed with ICE assistance with an international normalized ratio (INR) value of 1.86. Four vascular accesses were obtained by fellows in training: two right femoral and one left femoral venous accesses and one left femoral arterial access. A decapolar electrode catheter was positioned into the coronary sinus via the left femoral vein. An 8Fr ICE ViewFlex probe was than inserted into the left femoral vein and advanced to the inferior vena cava (IVC) through a 9Fr introducer, intended to carry towards the right atrium for image integration during CA. At that point, sudden abdominal pain was felt by the patient with associated hypotension and tachycardia.
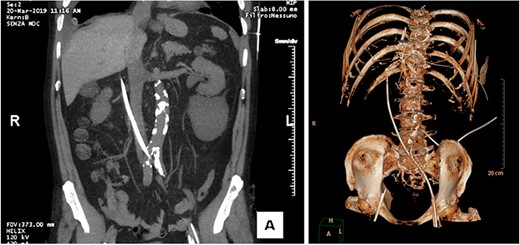
CT performed in urgency after catheter introduction shows the probe at the right side of the L2–L3 vertebral bodies, with the tip lying next to the portal vein.
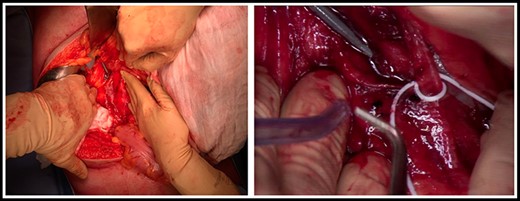
Intraoperative pictures showing the distal part of the probe outside the IVC.
Fluids and vasopressors (bolus of 500 ml of crystalloids, norepinephrine 0.1 mcg/kg/h) were administered to restore hemodynamic stability. Simultaneously, an abdominal FAST exam was performed with no evidence of intraperitoneal or pericardial free fluid, even if the location of the tip was unclear. Since the patient was hemodinamically stable, he was transferred for a thoraco-abdominal CT scan. Before, the decapolar electrode catheter was removed with concomitant administration of 3-factor prothrombin complex concentrate (1000 UI). As the patient was allergic to iodine, no contrast was injected. The CT scan revealed the distal part of the probe outside the IVC, at the L2–L3 vertebral level, and the tip free within the retroperitoneal space, near the portal vein, in absence of free fluid (Figure 1 a,b).
The IVC was injured by the passing probe. Since a strong traction of the probe could further tear the IVC with risk of uncontrolled hemorrhage, a surgical removal was planned and executed after informed consent was obtained from the patient.
Open repair was performed through a midline laparotomy. The Cattel-Braasch maneuver was carried out to expose the IVC. A retroperitoneal hematoma was observed anteriorly to the infrarenal IVC, without evidence of active bleeding. The IVC was prepared at the level of the left renal vein and at the bifurcation sufficiently to allow proximal and distal vascular control. The hematoma was then removed exposing the site of the perforation on the infrarenal IVC and the distal part of the probe outside the vein (Figure 2 a,b).
The probe was retracted under vision, the laceration was closed with a running 3-0 polypropylene suture and hemostasis was achieved by application of topical hemostatic agents. The abdomen was then closed in the standard fashion.
After 24 h anticoagulant medication with LMWH in therapeutic dose was safely reintroduced with a 48 h-delayed initiation of oral anticoagulation therapy. When target INR of 2–3 was achieved, LMWH was discontinued. The postoperative course was uneventful. The patient was discharged on eighth postoperative day, on oral anticoagulant medication.
At the 12-month follow-up, the patient was systematically well.
DISCUSSION
The acute complication rate of CA has decreased significantly in recent years due to the improved catheter technology and the growing experience, knowledge and expertise of the operators. Nevertheless, vascular complications remain the most common adverse events related to catheter-based CA likely due to the number and size of intravascular sheaths and the use of periprocedural anticoagulation. Retroperitoneal bleeding is fortunately rare and generally managed conservatively as most of vascular complications, but in some cases it may require administration of blood and surgical repair. Early recognition, especially if sudden hypotension develops during the procedure, is crucial and prompt actions must be taken to minimize the adverse consequences.
To our knowledge this is the first reported case of symptomatic IVC injury due to an ICE probe during CA.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



