-
PDF
- Split View
-
Views
-
Cite
Cite
Davide Esposito, Fabrizio Masciello, Walter Dorigo, Alessandro Alessi Innocenti, Raffaella Santi, Gabriella Nesi, Carlo Pratesi, An unexpected intraoperative finding of cystic adventitial degeneration of the common femoral artery, Journal of Surgical Case Reports, Volume 2020, Issue 8, August 2020, rjaa200, https://doi.org/10.1093/jscr/rjaa200
Close - Share Icon Share
Abstract
Herein we present a rare case of cystic adventitial degeneration involving the common femoral artery (CFA) of a 71-year-old patient, an unusual site of presentation of the disease. The most commonly affected district is the popliteal artery, and only a few cases of CFA involvement are described in literature. The history and comorbidities of the patient oriented us initially towards the diagnosis of an atherosclerotic obstructive disease. It was only intraoperatively indeed that a diagnosis of cystic adventitial arterial degeneration was made, subsequently confirmed by microscopic examination. Our case shows how both clinical and instrumental diagnosis of cystic adventitial disease can be challenging, given its non-specific presentation and low incidence. Suspicion of cystic adventitial degeneration is recommended in patients with sudden appearance of symptoms and with an isolated lesion of the affected artery without other involvement of the vascular tree.
INTRODUCTION
Cystic adventitial arterial degeneration is a very rare condition, which occurs mainly in the popliteal artery. Different locations of the disease, such as the common femoral artery (CFA) are instead extremely infrequent. In the present study, we report the case of cystic degeneration of the CFA which was diagnosed only at the operating table, and we try to suggest a therapeutic algorithm of this unusual condition.
CASE REPORT
A 71-year-old patient referred to our institution due to the sudden occurrence, 30 days earlier, of right thigh intermittent claudication, with a free-walking distance of about 50 m. The patient was a former artisan, suffering from hypertension, hyperlipidemia and diabetes. The symptoms were not attributable to recent traumatic events. At clinical examination, the right femoral pulse was present, while the popliteal and tibial pulses were absent, with an ankle-brachial index (ABI) of 0.6 on the right tibial arteries. The contralateral pulses were all present with an ABI value of 1. No signs of groin pulsatile mass were present.
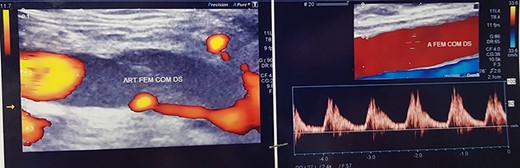
Duplex ultrasound examination (DUS, Fig. 1) showed a segmental sub-occlusive hypoechoic stenosis of the anterior wall of the right CFA.
![Angio CT images [1–4] and tridimensional reconstruction [5].](https://oupdevcdn.silverchair-staging.com/oup/backfile/Content_public/Journal/jscr/2020/8/10.1093_jscr_rjaa200/2/m_rjaa200f2.jpeg?Expires=1773458690&Signature=AO7DCHjY0k1~WRtWcFekoJ2RlFvJvqKxERp0lVV0iFMyeLgs47luUz7aX6QkGNrjs7XVi4Rkk0hvyermf3am7xlREAm3kJ-Sf6qXU-so~pVFJ61wFCaX~pQdpUuRdhz0EVNU0sxdO~OI0tzr8xnXgYDqcZ29xyUI5Ahk9Z3zbQ3Ht8ReMgYeWBtA~JaPbgv2o49hLK-m2KkHRlJN-1A25W7mx3Ly2ZlnztnVrVS2u8bI-~250a1GUyZDQPCMoft4XEaB8h6B3sjhNdUtu0EtMfnLmG2VfzRwUGD6fKAU2Ijp9Qrf92Sniiu8xMK3n3wAf6jtsKA1SzVmZ0d1VthCQQ__&Key-Pair-Id=APKAIYYTVHKX7JZB5EAA)
Subsequently, an angio computed tomography (CT) scan was carried out in order to make a more precise evaluation of the extension and etiology of the disease. A hypodense subocclusive segmental stenosis of the CFA was confirmed as the only critical lesion of the right lower limb arteries, without signs of advential involvement (Fig. 2). Therefore, a femoral thromboendarterectomy was planned and the informed consent for the treatment of personal data was acquired from the patient.
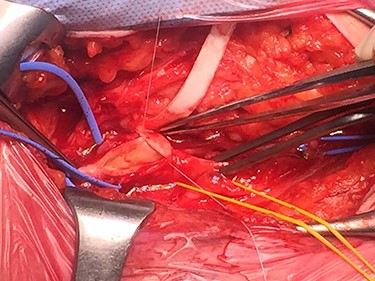
During surgical dissection of the right groin and isolation of the CFA, a jelly-like lesion of the anterior wall of the CFA was detected. The lesion caused a compression of the arterial lumen and determined its critical stenosis, with subsequent peripheral hypoperfusion leading to intermittent claudication. An accurate excision of the cystic material was performed and the clear gelatinous material leaked was collected along with a specimen of arterial wall for cytological and histological examination (Fig. 3). The surgical procedure was then completed with excision of the unhealthy arterial wall of the CFA and placement of a polyurethane patch.
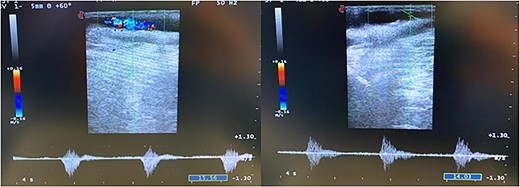
The intraoperative completion DUS showed the patency of the CFA and of the femoro-popliteal axis with triphasic flow maintained until tibial vessels (Fig. 4).
Microscopic examination of the surgical specimen demonstrated the presence of a cystic wall rimmed by paucicellular fibrocollagenic tissue, without evidence of an epithelial lining (Fig. 5).
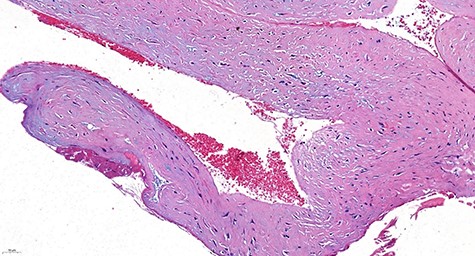
Histologically, the wall of the cyst consisted of paucicellular connective fibrous tissue. No epithelial lining was evident (H&E stain, ×20).
The patient was discharged on the third postoperative day with an ABI improved from 0.6 to 1.0 and complete remission of the symptoms.
| Etiologic theories of cystic adventitial degeneration | |
| Degenerative theory | A mucinous or myxomatous systemic degenerative condition associated with a generalized pathology. |
| Theory of repeated trauma | Repeated traumas could cause the destruction and cystic degeneration of the adventitia of the adjacent vessel. |
| Ganglia theory | Adventitial cysts arise as capsular structures which then tend to widen and spread along the vascular branches until they involve the adventitia of adjacent major vessels. |
| Theory of development | Mucin-secreting cells deriving from the mesenchyme of adjacent joints are erroneously positioned in the wall of a vessel during the development of the pathology. |
| Etiologic theories of cystic adventitial degeneration | |
| Degenerative theory | A mucinous or myxomatous systemic degenerative condition associated with a generalized pathology. |
| Theory of repeated trauma | Repeated traumas could cause the destruction and cystic degeneration of the adventitia of the adjacent vessel. |
| Ganglia theory | Adventitial cysts arise as capsular structures which then tend to widen and spread along the vascular branches until they involve the adventitia of adjacent major vessels. |
| Theory of development | Mucin-secreting cells deriving from the mesenchyme of adjacent joints are erroneously positioned in the wall of a vessel during the development of the pathology. |
| Etiologic theories of cystic adventitial degeneration | |
| Degenerative theory | A mucinous or myxomatous systemic degenerative condition associated with a generalized pathology. |
| Theory of repeated trauma | Repeated traumas could cause the destruction and cystic degeneration of the adventitia of the adjacent vessel. |
| Ganglia theory | Adventitial cysts arise as capsular structures which then tend to widen and spread along the vascular branches until they involve the adventitia of adjacent major vessels. |
| Theory of development | Mucin-secreting cells deriving from the mesenchyme of adjacent joints are erroneously positioned in the wall of a vessel during the development of the pathology. |
| Etiologic theories of cystic adventitial degeneration | |
| Degenerative theory | A mucinous or myxomatous systemic degenerative condition associated with a generalized pathology. |
| Theory of repeated trauma | Repeated traumas could cause the destruction and cystic degeneration of the adventitia of the adjacent vessel. |
| Ganglia theory | Adventitial cysts arise as capsular structures which then tend to widen and spread along the vascular branches until they involve the adventitia of adjacent major vessels. |
| Theory of development | Mucin-secreting cells deriving from the mesenchyme of adjacent joints are erroneously positioned in the wall of a vessel during the development of the pathology. |
At the 3- and 12-month DUS control, the patency of the treated vessel was confirmed.
DISCUSSION
Cystic adventitial disease, or cystic adventitial degeneration, was first described by Atkins and Key in 1947 [1]. This is an unusual non-atherosclerotic condition affecting peripheral vessels and consisting of a cystic tumor of blood vessels with accumulation of mucinous fluid inside the adventitia. Young men are commonly affected, while its presentation at an older age is less common.
Symptoms occur when the cystic adventitial degeneration determines a progressive external compression and subsequent stenosis of the vessel lumen, leading to symptoms such as claudication and swelling of the limb when venous compression occurs. It is estimated that the incidence of this disease is one in 1200 cases of intermittent claudication [2].
In the clinical case herein presented, both the patient’s advanced age and the various atherosclerotic risk factors drove towards the diagnosis of peripheral artery disease.
A systematic review by Lejay and Ohana [3] collected more than 700 cases of cystic adventitial degeneration described in literature. In the great majority (>90%), the degeneration involved peripheral arteries, with isolated cases of venous interest or involvement of both districts. The most common site is the popliteal artery (~90% of cases), followed by femoral arteries (~6%), radial artery (~3%), external iliac artery and axillary artery.
The pathogenesis of this condition is still not completely clear. Articles by Schramek et al. [4] in 1973 and Flanigan et al. [5] in 1979 suggested four possible etiologies, resumed in Table 1.
Nowadays, the most accredited hypothesis seems to be the ganglia theory [6].
Imaging tests play a major role in the diagnosis of this disease. DUS and magnetic resonance have been identified as the most specific techniques for the diagnosis of the liquid nature of the lesion and the anatomic connection with the arterial wall [7].
The literature reports different surgical therapeutic options, ranging from echo-guided aspiration of the cyst or traditional open excision, to patch angioplasty, graft interposition or bypass with or without cyst excision [8].
Percutaneous aspiration of the cyst and angioplasty with stent placement have shown unsatisfactory results and a high rate of recurrence [9].
In a retrospective multi-institutional study, Raghu and Motaganahalli [10] analyzed treatment options and outcomes of 47 patients affected by the disease. The most commonly performed surgical procedure was cyst resection combined with interposition of a venous graft, but the best option in terms of symptoms relief and freedom from reintervention was bypass grafting, with or without cyst excision.
In our case, given the scarce circumferential and longitudinal involvement of the cystic degeneration of the CFA, after being sure of both having completely removed the lesion and warranting a sufficient healthy wall, we opted for an angioplasty with patch interposition. Our main concern about the procedure is the possible recurrence of a new cystic degeneration related to the possible incomplete excision of the affected arterial wall. However, at the time of writing, after the 3- and 12-month follow-up DUS examinations, no new cystic formation was identified. Our belief is that an accurate excision of the degenerated tissue could be the key point for a durable repair without exacerbation of the disease. Furthermore, lesion removal combined with patch angioplasty represents the less invasive effective procedure for segmental lesions, with short hospitalization and prompt recovery of quality of life.
AUTHOR CONTRIBUTIONS
All authors have seen and approved the final version of the manuscript. The article is the authors’ original work, has not received prior publication and is not under consideration for publication elsewhere.
CONFLICT OF INTEREST
The authors have no conflicts to disclose.



