-
PDF
- Split View
-
Views
-
Cite
Cite
Stefan F Lange, Tim K J Schrooten, Ralph J de Wit, Reinier de Groot, A hybrid treatment modality of a subtrochanteric femoral fracture in a patient with osteoporosis due to a renal Fanconi syndrome: a case report, Journal of Surgical Case Reports, Volume 2020, Issue 8, August 2020, rjaa130, https://doi.org/10.1093/jscr/rjaa130
Close - Share Icon Share
Abstract
A 24-year-old male with an idiopathic renal Fanconi syndrome presented to our ER after a low-energetic fall. Conventional imaging revealed a right subtrochanteric femoral fracture, severely decreased bone quality and cannulated collum femoris screws on the contralateral side. Regular plate-screw osteosynthesis or cephalomedullary implantation was deemed insufficient, due to a high iatrogenic and periprosthetic fracture probability. The decision was made to perform a plate-screw osteosynthesis combined with an intramedullary polymer bone enhancement (IlluminOss), to minimize this risk. No complications occurred perioperatively. The patient was able to walk independently two months postoperatively. This case shows that use of polymer implant as an enhancement of osteosynthesis in repair of fractures in the Fanconi syndrome is a safe and possible useful treatment method.
INTRODUCTION
Renal Fanconi syndrome is a disorder in which tubular dysfunction may lead to electrolyte disturbances. One of the frequently excreted electrolytes is phosphorus. Hypophosphatemia in turn may cause rickets in children, or osteomalacia in adults. We present a 24-year-old Caucasian male with idiopathic renal Fanconi syndrome who fell and presented to the emergency room at our regional level A-trauma centre.
CASE REPORT
The patient was haemodynamically stable at presentation. He complained about pain in his right hip and was not able to move his right leg due to the pain. The patient was previously diagnosed with the renal Fanconi syndrome and had a previous collum femoris fracture on the left side. Conventional imaging revealed a subtrochanteric femoral fracture (Figs 1 and 2). Furthermore, contralaterally placed cannulated collum femoris screws and a severely decreased bone quality was found. No other traumatic injuries were present. Biochemical analysis showed a hypokalaemia of 3.0 mmol/l (3.5–5.0 mmol/l) and a mild hyponatraemia of 134 mmol/l (135–145 mmol/l). These findings can be related to the Fanconi syndrome.
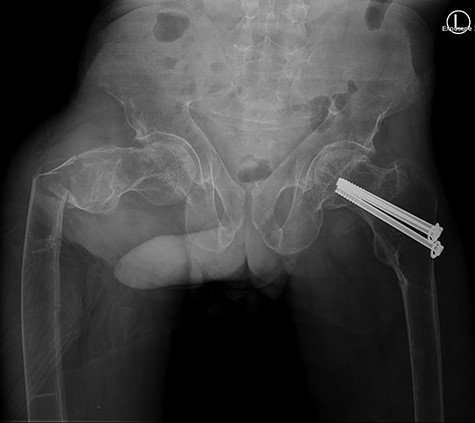
Anterior-posterior view: right-sided subtrochanteric femoral fracture, left-sided collum femoris screws.

Surgical considerations
Regular or extended cephalomedullary nail implantation was deemed inadequate, due to the poor bone quality and thereby an increased risk of iatrogenic fracturing. The wide marrow cavity combined with a poor cortex would possibly result in an unstable nail position and increased risk of a periprosthetic fracture. A dynamic hip screw (DHS) alone would not have enough grip for its screws due to the lack of bony cortex. We decided to combine intramedullary polymer bone enhancement (IlluminOss) with a DHS osteosynthesis. The IlluminOss would create enough grip for the DHS to form a stable biomechanical situation and decrease risk of a periprosthetic fracture.
Surgery
The patient was placed in a supine position on a fracture table. Spinal anaesthesia was performed and combined with sedation. Traction was applied and fluoroscopy confirmed adequate position of the fracture fragments. Surgical site was disinfected and draped. A trochanteric incision was performed, the fascia was opened and soft tissues were bluntly dissected until the greater trochanter was visible. Bone quality was poor and bone fragments were easily bended manually. Bone fragments were further repositioned and a Kirschner wire was placed at the collum femoris screw site using the aiming device. A prime was used to create the introduction site for the IlluminOss on the trochanteric tip. A guide wire was advanced and adequate position was confirmed by fluoroscopy. Introduction site was reamed with a 6.5 mm reamer. The sheath and balloon were prepared extra corporally and hereafter introduced into the femoral shaft using the guidewire. Hereafter, guidewire and sheath were removed and monomers were infused. Fluoroscopy showed adequate expansion of the balloon. Monomers were hardened for 1000 s with IlluminOss, after which the balloon was cut at the trochanteric tip. The collum screw site was drilled along the previously placed Kirschner wire and a 85 mm collum screw attached to a 4-hole omega3 plate was placed. The plate position was slightly rotated longitudinally due to pre-existent deformation of the femur. Four screws were placed, of which the one above the fracture site was used as a pulling screw. An adequate position was achieved. The surgical site was closed in layers after extensive lavation.
Postoperative
Our patient was discharged from the hospital 14 days after the surgery. The long hospital stay was mostly due to the management of the renal Fanconi syndrome. He was able to mobilize with crutches at time of discharge. The in-hospital stay was without complications. Eight weeks postoperatively our patient returned to our outpatient clinic. Full mobilization was possible and there was a full range of motion. Conventional imaging showed an adequate position of our hybrid osteosynthesis (Fig. 3) and an almost completely healed fracture site.
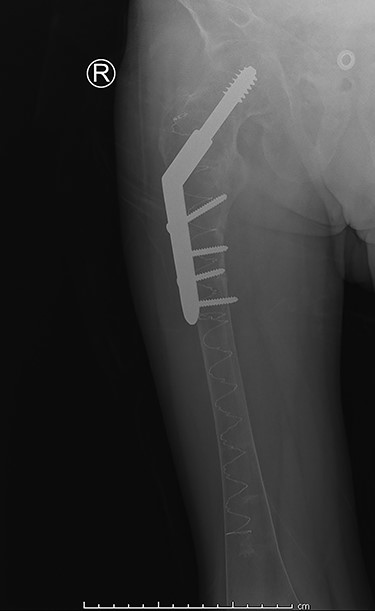
Post-operative anterior–posterior view: DHS osteosynthesis with intramedullary bone enhancement.
DISCUSSION
The aim of (osteoporotic) fracture treatment is function maintenance, even if anatomical position is lost [1]. Cephalomedullary nails are considered to be the best treatment option in unstable subtrochanteric fractures, when compared to other fixation techniques [2]. This is due to the central position of the cephalomedullary nail combined with impaction of the fracture [3].
In this case, we decided against a cephalomedullary device, due to the poor bone quality of the femur and the concomitant high risk of iatrogenic fracturing. Therefore, we reinforced the femoral shaft using Illuminoss before fixation with a DHS. This fixation is comparable to traditional intramedullary fixation [4]. Placement of the omega 3 implant was possible, due to the immediate stability that the polymer provides. This combination of reinforcing with Illuminoss and fixation with the omega 3 implant provides the same biomechanical benefits as a traditional cephalomedullary device.
This technique has only recently been developed. To our knowledge, this is the second case in which regular osteosynthesis implants are combined with intramedullary polymer bone enhancement for patients with osteomalacia [5]. This treatment modality should be considered in patients with poor bone quality and fractures of major, weight-bearing bones.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
This research did not receive any specific grant from funding agencies in the public, commercial or not-for-profit sectors.



