-
PDF
- Split View
-
Views
-
Cite
Cite
Almog Ben-Yaacov, Nikolay Menasherov, Vyacheslav Bard, Repair of a recurrent symptomatic hernia through the foramen of Morgagni: a case study and review of the literature, Journal of Surgical Case Reports, Volume 2020, Issue 7, July 2020, rjaa230, https://doi.org/10.1093/jscr/rjaa230
Close - Share Icon Share
Abstract
The prevalence and natural history in adults of Morgagni hernias have been relatively poorly characterized. A case is presented of a 31-year-old man where the hernia recurred following a laparoscopic mesh repair. In the era of minimally invasive surgery, debate concerns whether the peritoneal sac should be excised and if the insertion of mesh is superior to primary diaphragmatic repair.
INTRODUCTION
An anterior hernial defect between the sternal and costal diaphragmatic attachments was first described by Giovanni Battista Morgagni (1682–1771) in 1769 [1]. The defect represents a natural separation in the embryological diaphragmatic elements of the peripheral muscle (pleuroperitoneal folds) and the central tendon (septum transversum). The position of anterior or anteromedial subcostal/substernal diaphragmatic hernias permits soft tissues and viscera to enter the thorax; the hernia usually contains omentum but also on occasion colon, liver and even stomach. These hernias may also include those listed as retrocostoxiphoid, parasternal, retrochondrosternal, retrosternal, subcostal, substernal and subcostosternal.
Hernias of Morgagni account for only 3% of all surgically treated diaphragmatic cases showing a predilection for females. Over 90% are right-sided with one-quarter symptomatic [2]. The increased use of computed tomography (CT) scanning in the evaluation of surgical disease and the rise of minimally invasive technology has changed management. There are few reports in the literature concerning the prevalence and natural history of this condition with repair advocated because of the risk of strangulation of herniated contents [3]. A range of surgical repair options has been used with a recent emphasis on minimally invasive (laparoscopic, thoracoscopic and robotic) approaches [4–6]. We present the laparoscopic management of a case with a review of the literature.
CASE REPORT
A 31-year-old male with Down’s syndrome presented with repeated hospital admissions over the previous year complaining of upper abdominal pain, nausea, postprandial vomiting and 10 kg weight loss. In 2004, he had undergone a previous laparoscopic repair of a Morgagni hernia with mesh insertion at our institution but was lost to follow-up. Past medical history included a Ventricular septal defect (VSD) repair, Atrioventricular (AV) block with pacemaker insertion and hypothyroidism. A chest X-ray (Fig. 1) showed right middle lobe consolidation, and a thoracoabdominal CT demonstrated the mesh located in the anterior thorax, which contained colon without any features of ischemia (Fig. 2). Gastroscopy and colonoscopy were normal.

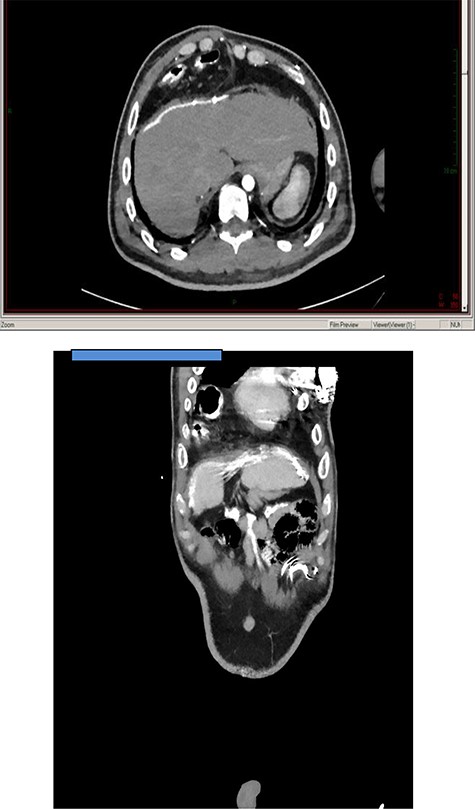
Axial and coronal thoracoabdominal CT showing transthoracic displacement of a segment of colon covered by the old mesh implant.
SURGICAL TECHNIQUE
The patient was placed in a reverse Trendelenburg position with the legs apart and the operating surgeon seated between the legs. A 12-mm trochar was placed above the umbilicus with pneumoperitoneum established by Hasson’s technique. One 5-mm trochar was placed in the right upper quadrant with another 5-mm trochar inserted into the left upper quadrant. A 12-mm working trochar was positioned in the epigastrium. The falciform ligament was divided for access to the diaphragmatic defect. Both the transverse colon and omentum were adherent to the hernial sac but without incarceration. The mesh was closely adherent to the hernial sac and the liver (Fig. 3). Following adhesiolysis using the harmonic scalpel, the colon was reduced into the abdomen without excessive dissection of the medial aspect of the hernial sac. The hernial defect was measured at 12 × 10 cm with primary closure considered unsuitable with a decision made for mesh insertion using a 10 × 15 cm onlay Parietex™ Optimized Composite mesh (Covidien, Minneapolis, MN). There was a 3–5 cm overlap beyond the edges of the defect. The mesh was secured by fixation (AbsorbaTack™ Covidien). Figure 4 shows the measurement of the defect and the onlay mesh insertion. The operative time was 150 minutes. The postoperative recovery was uneventful, with the patient commencing a clear liquid diet by the first postoperative day and a regular diet the day after. He was discharged on the fourth postoperative day and at 30 days follow-up was asymptomatic, eating a normal diet and having gained 3 kg in weight.

Laparoscopic views of the defect and attendant omental adhesions.

Ruler measurement (top image) and mesh overlap onlay (bottom image).
DISCUSSION
Most studies concerning the management of Morgagni-type hernias have been reported in the paediatric literature. As in our case, about one-third of adults present with abdominal or thoracic pain and a range of other gastrointestinal symptoms. Gastroesophageal reflux and dysphagia are uncommon [5]. The hernia size does not seem to correlate with symptoms [2], with colon and/or omentum the most common hernial contents [7]. In 1993, Kuster et al. [8] first reported a laparoscopic repair of a Morgagni hernia, with Rau et al. [9] first describing the use of synthetic mesh interposition the following year. The majority of reports using minimally invasive approaches are either individual cases or small case series with a suggested advantage in the laparoscopic or robotic abdominal approach over thoracoscopic repair [10]. Laparoscopy permits evaluation of the contralateral diaphragm as well as examination of the remainder of the abdomen and ready reduction of the hernial contents. A decision is made to use a mesh inlay for larger defects, although the optimal mesh type is at present unclear. Concerning the laparoscopic decision for mesh, Ryan et al. [4] reported primary closure of the defect in 34.5% of cases, primary closure plus mesh reinforcement in 14.1% and mesh interposition primarily in 49.6% of patients, with a recommendation for the use of mesh only if the hernial defect exceeds 20–30 cm2 in area.
Although controversial, we do not perform complete excision of the hernial sac preferring extrasaccular dissection to better define the mediastinal structures. We accept that this represents a balance between recurrence and mediastinal structural injury [11] and that sac excision tend to be less commonly performed via a laparoscopic approach when compared with open surgery [2]. If medial excision of the sac is avoided, there is a reduced risk of injury to a range of structures including the lung, pleura, pericardium, superior epigastric vessels and the phrenic nerve. Care should also be taken near the edge of the defect during helical tack fixation since the diaphragm at this point can be exceedingly thin. In summary, repeat laparoscopic treatment of a hernia of Morgagni is safe and efficient. It is accepted that our follow-up period in this case is short with the central debate over whether to partially excise the hernial sac and when to primarily repair the defect.
FUNDING
None declared.
ETHICAL APPROVAL
Not applicable.
TRIAL REGISTRY NUMBER
Not applicable.
AUTHOR CONTRIBUTION
V.B. contributed to the concept and design of the case, operator of the patient, data interpretation and analysis, drafting and approval of the final manuscript.



