-
PDF
- Split View
-
Views
-
Cite
Cite
Maura Morgan, Timothy Farrell, Gordian U Ndubizu, Timothy J Farrell, Colonic lavage in treatment of refractory Clostridium difficile infection: an adaptation of the Pittsburgh protocol, Journal of Surgical Case Reports, Volume 2020, Issue 7, July 2020, rjaa159, https://doi.org/10.1093/jscr/rjaa159
Close - Share Icon Share
Abstract
Clostridium difficile infection (CDI) is a common nosocomial sequela in patients treated with antibiotics. Surgical intervention is indicated in fulminant cases. However, the mortality associated with total colectomy and end ileostomy is high. Previous reports have indicated that surgical intervention for severe complicated CDI with formation of a loop ileostomy leading to the diversion of fecal stream followed by colonic lavage can be beneficial in treating severe CDI. This procedure is known as the Pittsburgh protocol and has been reported to decrease the mortality and the need for a total colectomy in patients with severe complicated CDI. In this case, we present a 75-year-old female with refractory CDI. In her treatment, we adapted the Pittsburgh protocol and utilized a 20-French MIC gastrostomy tube to recreate the ileocecal valve and control the colonic lavage without retrograde flow.
INTRODUCTION
Clostridium difficile, the culprit of antibiotic-associated pseudomembranous colitis, is an anaerobic Gram-positive cytotoxin-producing bacteria [1]. C. difficile infection (CDI) is the leading cause of healthcare-associated infections in the United States. As many as 500 000 infections occur annually. Manifestations vary from nonsevere to fulminant disease [2]. Up to 10% of patients have disease progression despite appropriate antimicrobial therapy. In patients who progress to fulminant disease total abdominal colectomy with end ileostomy is the standard of care. However, this has been called into question since McCreery et al. published their results with fecal diversion and antegrade colonic lavage, the ‘Pittsburgh protocol.’ Standard surgical intervention in those with fulminant disease is associated with a 30 day mortality of up to 71% [3]. For this reason, many advocate for early surgical intervention with total abdominal colectomy as opposed to waiting for the development of fulminant disease.
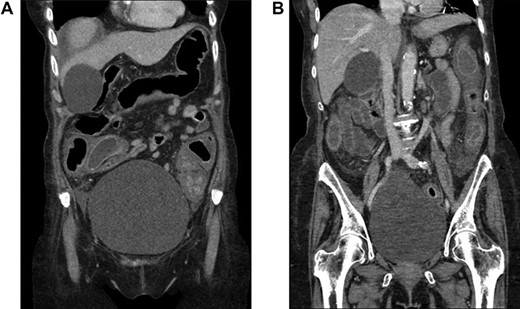
CT scan of the abdomen and pelvis demonstrating pancolitis from CDI.
Although earlier surgical intervention leads to improved outcomes, it remains unclear what constitutes the optimal time for surgical intervention. Currently accepted indications for surgery in those with CDI includes, hemodynamic instability, megacolon, perforation or need for intensive care unit admission [4]. Furthermore, Klobuka et al. established the following as parameters for early surgical intervention: age greater than 65, peritoneal signs on physical examination, abdominal distension, end-organ failure, systolic blood pressure less than 90 mm Hg, heart rate greater than 100 beats per minute, need for vasopressor, leukocytosis of greater than 16 × 109/μl, serum lactate of greater than 2.2 mmol/l and radiographic findings of pancolitis, ascites, megacolon or colonic perforation [5].
The advent of the Pittsburgh protocol in 2017 in conjunction with an emphasis on earlier surgical intervention has led to a re-evaluation of the use of total abdominal colectomy in the treatment of severe CDI. Fecal diversion with diverting ileostomy disrupts the fecal stream, deprives the intestinal flora of nutrition and decreases the colonic toxin burden. In the pilot study by McCreery et al., individuals that met the diagnostic criteria for severe or fulminant CDI and were surgical candidates underwent a diagnostic laparoscopy and creation of a loop ileostomy. Subsequently, 8 l warmed polyethylene glycol 3350/electrolyte solution was introduced through the distal end of the ileostomy and collected via a rectal drainage tube. Postoperatively, the patient received antegrade vancomycin flushes, 500 mg in 500 ml lactated ringers every 8 hours, via a Malecot catheter (24 French) left in the efferent limb of the ileostomy, and 500 mg IV metronidazole every 8 hours for 10 days. The reported mortality for these patients was 19% in the immediate postoperative period. An additional 14% died outside of this time frame of which none of the deaths were related to CDI. Of note, 3 of the 43 patients who underwent diversion required conversion to total abdominal colectomy [6]. Here we describe a case of severe CDI managed successfully with slight modification of the original protocol.
CASE REPORT
A 75-year-old female presented to the hospital exactly 1 month following a prior hospital admission in which methicillin-resistant Staphylococcus aureus pneumonia was diagnosed and treated with IV vancomycin for 9 days. Four days prior to readmission, she was diagnosed with CDI and had symptoms of fever, nausea, vomiting and diarrhea. Her WBC was 22 860 cells per cubic millimeter (CCM) of blood, and PO vancomycin and IV metronidazole were initiated upon admission. At that time, a CT scan of the abdomen and pelvis was obtained and showed severe pancolitis consistent with CDI (Figure 1). Within 2 days, she became increasingly hemodynamically unstable with a leukocytosis of 38 680 cells per CCM. Due to severe CDI on appropriate medical therapy, surgical intervention was deemed necessary.
A laparotomy was performed, and the large and small bowel deemed viable. Subsequently, a loop ileostomy was fashioned and a 20-French MIC gastrostomy tube advanced through the efferent limb with the balloon inflated just beyond the ileocecal valve. The colon was lavaged with GoLYTELY solution as per the initial Pittsburg protocol, and the patient transitioned to the intensive care unit following abdominal wall closure.
On postoperative day zero antegrade vancomycin lavage was performed through the ostomy. Lavages were continued until postoperative day 12. Leukocytosis resolved on the 4th postoperative day. The patient was deemed stable for discharge by postoperative day 15. Three months later, the patient underwent uneventful reversal of the ileostomy in a handsewn manner and is currently awaiting repair of an incisional hernia at her previous stoma site.
DISCUSSION
Antibiotic-associated pseudomembranous colitis due to C. difficile is a common nosocomial infection in the setting of recent antibiotic use. Even with medical therapy, 10% of cases progress leading to eventual hemodynamic instability and death if not appropriately treated. It is paramount to have protocols in place for refractory cases. The Pittsburgh protocol presents an alternative to the current gold standard in surgical intervention, in this patient population. One significant modification from the original protocol was performed in our case study.
A MIC gastrostomy tube was placed in the efferent limb of the ostomy instead of a Malecot drain. Antegrade vancomycin lavage was performed through this route and led to resolution of the patient’s leukocytosis in 4 days. We preferred use of the 20-French MIC gastrostomy tube as it allows for recreation of the ileocecal valve. Furthermore, balloon inflation ensured a water-tight seal such that all administered enteric/colonic vancomycin remained within the gastrointestinal tract. No antibiotics were lost due to spillage or retrograde flow of colonic contents. This is of importance in those with pseudo-colonic obstruction caused by severe or fulminant colitis. Additionally, this route of administration is more efficient than that described in the original proposal.
The high mortality rate associated with total abdominal colectomy in the treatment of severe CDI necessitates improvement in our current treatment protocols. This case highlights the use of colonic diversion and lavage as an alternative to the current gold standard. Continued review is required to formulate the optimal treatment algorithm and optimize patient outcomes.
CONFLICT OF INTEREST STATEMENT
None declared.
FUNDING
None.



