-
PDF
- Split View
-
Views
-
Cite
Cite
Edward R Hagen, Nathan Hite, John Griffin, Rodney Kratz, Perianal basal cell carcinoma: a common cancer in an uncommon location, Journal of Surgical Case Reports, Volume 2020, Issue 7, July 2020, rjaa151, https://doi.org/10.1093/jscr/rjaa151
Close - Share Icon Share
Abstract
This is a case of a perianal basal cell carcinoma, a common skin cancer in an unusual location. Our patient is a 67-year-old male with a perianal lesion. He first noticed this painless lesion 5 years prior to presentation and was having fecal incontinence and weight loss. He had a fully encompassing ulcerated lesion involving the entirety of the anal margin. We performed a biopsy that returned on pathology as a basal cell carcinoma. Due to the size of the lesion and his current nutritional status, it was determined to be unresectable. We were able to provide him with a diverting colostomy to address his incontinence and this allowed the patient to recover enough to undergo treatment with radiation (total of 5400 cGy). To our knowledge, this is the largest perianal basal cell carcinoma reported in the literature and an example of combining palliative surgery and radiation as a treatment option.
INTRODUCTION
Basal cell carcinoma (BCC) is a very common skin malignancy, making up 80% of the nonmelanoma skin cancers [1]. Its classic presentation is an erythematous patch of scaly skin that may or may not contain melanin. BCC is due to inappropriate activation of the hedgehog signaling pathway and mutations of the p53 tumor suppressor gene is found in half of the cases [2]. These mutations are secondary to ultraviolet (UV) radiation, which correlates with the risk factors being tanning bed use, light skin color and exposure to UV light. For that reason, it is very uncommon to find this pathology in areas not exposed to the sun, such as the perianal region [3].
The largest review of perianal and genital BCC’s was completed by Gibson et al. It consisted of 51 cases with only 15 perianal lesions. The average size was 1.95 cm and the majority of patients were treated with wide local excision (WLE) [4]. The largest lesion to our knowledge was reported in 2002 by Damin et al. and was an 8 × 5 cm lesion also treated with WLE [5].
CASE REPORT
Our patient is a 67-year-old gentleman who presented to our emergency department after a ground level fall. During his workup for the fall, he complained of fecal incontinence and a painful lesion in his perianal area. The patient first noticed the lesion 5 years prior to his presentation and approximately 3 years ago he also began having fecal incontinence with occasional bleeding. He has a history of multiple BCC’s of the arms and face as an adolescent but has not sought medical care for decades.
The perianal lesion encompassed the entirety of the anal margin. It had scalloped edges along the periphery of the lesion with a pale pink wound bed and associated mucoid drainage. There was no anorectal tenderness on exam but also no sphincter tone. The mass measured 11 × 6 cm with a 2 cm extension into the anal canal (Fig. 1).

Multiple 4-mm punch biopsies were obtained which returned as BCC with nodular and infiltrative patterns. A computed tomography of the chest abdomen and pelvis was obtained that showed no evidence of metastatic disease. A magnetic resonance imaging (MRI) of the pelvis (Fig. 2) showed extension into the anal canal with complete loss of the external sphincter muscle and a majority of the internal sphincter muscle.
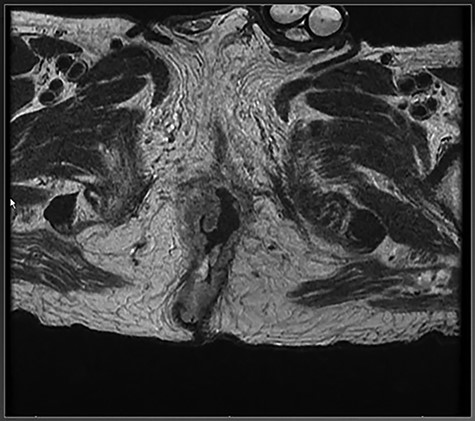
MRI of pelvis showing extension of tumor through the right external sphincter.
The patient’s treatment options were discussed amongst our colorectal surgical team. Due to the extent of the disease and the patient’s poor health and nutrition at baseline a complete resection was not deemed possible. We instead performed a diverting colostomy for control of the incontinence followed by palliative radiation therapy.
He completed 10 rounds of radiation and due to pain associated with his palliative radiation therapy and ongoing insecurities of his wound he declined further follow-up or evaluation of his wound.
DISCUSSION
BCC is a common skin malignancy but perianal BCC is rarely reported in the literature due to its very low incidence. It is typically treated with surgical excision and recurrence rates are <5% if negative margins are obtained [6]. Alternatives to surgical excision include topical immunomodulators such as imiquimod or fluorouracil and in this case radiation. The surgical reports of perianal BCC in the literature have been treated with Mohs micrographic surgery (MMS)—with no recurrence at one-year follow-up [7]. Larger lesions have been treated with a WLE and reconstruction using a V-Y advancement flap [8]. A nonoperative approach was taken for a smaller sized lesion in a poor surgical candidate. This patient was treated with 6 weeks of radiotherapy with success [6].
Perianal BCC is an uncommon anorectal pathology but important to remember as part of the differential diagnosis for perianal lesions. Once diagnosed, it is imperative to involve a multidisciplinary team to utilize all treatment options available for the best outcome of the patient. This case report is to our knowledge the largest perianal BCC in the literature and shows how palliative surgery combined with radiation can be used as treatment.
CONFLICT OF INTEREST
None declared.
Disclaimers: No disclaimers.
Sources of Support: No sources of support.
Future/Past Presentations of the manuscript: Manuscript has not been accepted as a presentation or poster.



