-
PDF
- Split View
-
Views
-
Cite
Cite
Daniele Bernardi, Davide Ferrari, Stefano Siboni, Matteo Porta, Barbara Bruni, Luigi Bonavina, Minimally invasive approach to esophageal lipoma, Journal of Surgical Case Reports, Volume 2020, Issue 7, July 2020, rjaa123, https://doi.org/10.1093/jscr/rjaa123
Close - Share Icon Share
Abstract
Esophageal lipoma is a rare neoplasm with heterogeneous and sometimes life-threatening clinical presentation. We report the case of two patients, a 77-year-old man and a 69-year-old woman presenting with heartburn and dysphagia, and with recurrent vomiting and asphyxia, respectively. Upper gastrointestinal endoscopy and computed tomography were highly suggestive of the diagnosis of esophageal lipoma and identified an intramural and an intraluminal pedunculated mass originating, respectively, from the distal and the cervical esophagus. The first patient was treated by laparoscopic transhiatal enucleation and the second by transoral endoscopic resection under general anesthesia. Both had an uneventful postoperative course and were discharged home on postoperative day 2. Minimally invasive excision of esophageal lipoma is feasible and effective. It may be life-saving in patients with pedunculated tumors who suffer from intermittent regurgitation of a bulky polypoid mass in the mouth causing asphyxia.
INTRODUCTION
Lipoma accounts for 0.4% of benign tumors of the esophagus, which represent <1% of all esophageal neoplasms coming to clinical attention [1]. Esophageal lipoma occurs mostly in male patients, with a 2:1 male to female ratio [2], and can present as intramural lesions or as pedunculated tumors with a long stalk covered by normal mucosa. In a previous review of the literature, 16 of 17 esophageal lipomas were intraluminal, most frequently arising from the cervical esophagus, and causing respiratory distress symptoms and possible death by asphyxia [3–4].
The majority of esophageal lipomas are found incidentally during upper gastrointestinal endoscopy. The most commonly referred symptoms are dysphagia, heartburn and/or regurgitation leading to an initial clinical suspicion of esophageal malignancy, achalasia, or hiatus hernia [5]. Surgical or endoscopic intervention is often required, and various techniques have been described including excision of the mass and, more rarely, esophagectomy [6, 7]. We describe a successful minimally invasive approach in two patients with a proximal and distal esophageal lipoma recently treated at our institution.
CASE 1
A 77-year-old man was referred for a long history of heartburn and more recent onset of progressive regurgitation, dysphagia and weight loss. Empirical therapy with proton-pump inhibitors was ineffective. The gastroesophageal reflux disease health-related quality of life (GERD-HRQL) score was 22. The functional outcome swallowing scale (FOSS) score for dysphagia was 2. Physical examination was unremarkable. Upper gastrointestinal endoscopy showed a soft submucosal bulging in the posterior wall of the distal esophagus located between 29 and 39 cm from the incisors, and 3 cm proximal to the esophago-gastric junction (Fig. 1). Computed tomography of chest and abdomen showed a fat-density submucosal mass with luminal narrowing (Fig. 2). High resolution manometry (HRM) showed pan-esophageal pressurization in 100% of the swallows and a resting lower esophageal sphincter (LES) pressure of 11.2 mmHg (Fig. 3). Through a laparoscopic transhiatal approach, esophageal myotomy, mass enucleation, suture approximation of the muscle layer, posterior cruroplasty, and 270° Toupet fundoplication was performed (Fig. 4). The procedure took 55 min. Postoperative course was uneventful. A gastrographin swallow study on Day 1 showed a normal esophagogastric transit and the absence of leaks. The patient was discharged home on postoperative Day 2. Pathology confirmed the clinical suspicion of esophageal lipoma (Fig. 5). High-resolution manometry was repeated at the 6 month follow-up and showed an ineffective esophageal motility, with 50% of non-conducted swallows. The resting LES pressure increased (17.4 mmHg), and the swallow-induced LES relaxation was normal. The GERD-HRQL score was 3 and the FOSS score was 0.

Upper gastrointestinal endoscopy showing submucosal lipoma of the distal esophagus extending between 29 and 39 cm from the incisors.
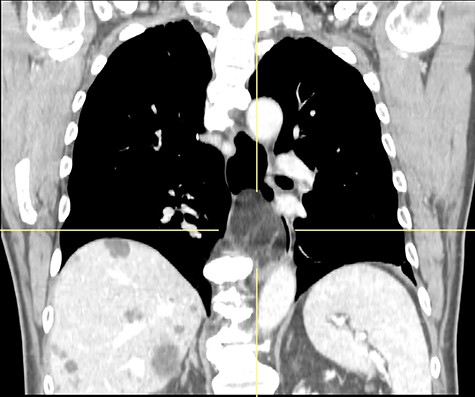
CT scan showing fat-density submucosal mass with luminal narrowing.
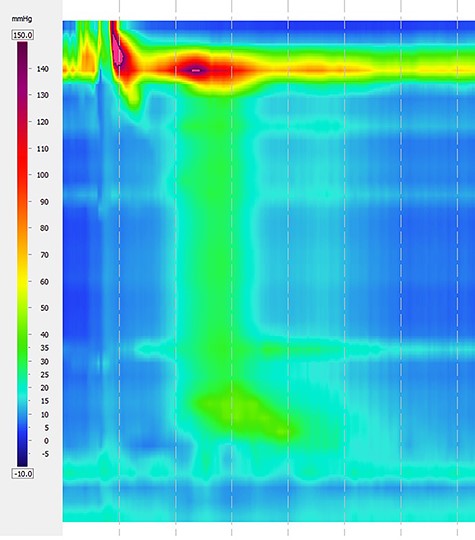
Pre-operative high-resolution manometry showing pan-esophageal pressurization in 100% of the swallows.

Laparoscopic transhiatal enucleation of an intramural distal esophageal lipoma.
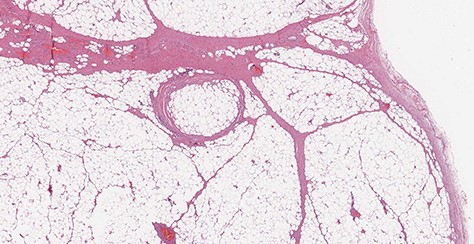
Microscopic transverse section revealing a benign tumor composed of a large amount of mature adipocytes with a flat peripheral nucleus without atypia, surrounded by fibrous tissue and containing rare blood vessels (H&E stain, ×10).
CASE 2
A 69-year-old woman was referred because of recurrent episodes of vomiting with concomitant regurgitation of a fleshy mass in the mouth and multiple episodes of asphyxia. The patient had a long history of heartburn and a GERD-HRQL score of 18. An upper GI endoscopy revealed a long pedunculated polypoid mass covered with normal squamous epithelium (Fig. 6). A computed tomography (CT) scan showed a fat-density mass in the esophageal lumen, originating about 1 cm below the upper esophageal sphincter and extending caudally in the esophageal lumen. A flexible endoscopic procedure was performed under general anesthesia and orotracheal intubation. An endoclip was placed at the base of the stalk in the cervical esophagus, and a snare resection of the pedunculated lipoma was successfully performed (Fig. 7). The procedure lasted 40 min. The patient began a soft diet on postoperative Day 1, which was well tolerated, and was discharged home on postoperative Day 2. Pathology confirmed a preponderant component of adipose tissue with a central fibrovascular core, covered by normal esophageal squamous mucosa (Fig. 8). At the 3 month follow-up visit the patient was asymptomatic, with a GERD-HRQL of 5 under treatment with proton-pump inhibitors.
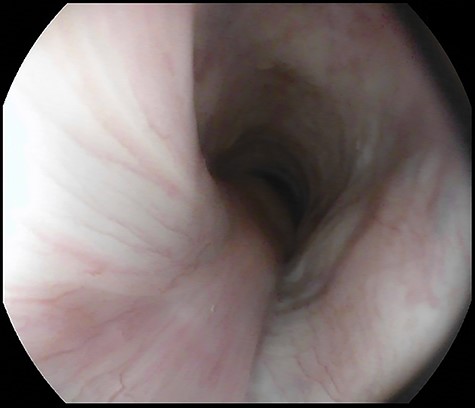
Pre-operative upper gastrointestinal endoscopy showing pedunculated lipoma arising 1 cm below the upper esophageal sphincter and extending from 18 to 26 cm from the incisors.

Operative specimen of the pedunculated esophageal lipoma measuring 8 × 3.5 cm.

Microscopic transverse section of the pedunculated lipoma composed by mature adipocytes, interspersed by blood vessels, surrounding a central fibrovascular axis; Tumor covered by intact esophageal squamous mucosa. No spindle cells are present. (H&E stain, ×4).
DISCUSSION
Lipoma is an uncommon benign esophageal tumor. Intraluminal neoplasms have often been reported as fibrovascular polyps. However, a significant component of adipose tissue is generally found at pathologic examination [8]. Liposarcoma has rarely been reported [9]. Heartburn and/or dysphagia are common symptoms in patients with esophageal lipoma. In our first patient, HRM showed partial recovery of esophageal peristalsis after laparoscopic surgery possibly related to mass enucleation and fundoplication. In both patients, the GERD-HRQL score decreased postoperatively. A unique clinical presentation of the pedunculated lipoma is regurgitation of the mass in the mouth leading to asphyxiation and possible death. Interestingly, in the literature review by [6], seven fatalities occurred among 110 observed patients.
The surgical approach to esophageal lipoma has been heterogeneous, generally through an open cervicotomy or thoracotomy, depending on the anatomical location. An esophagectomy has seldom been reported in patients with very giant lesions or liposarcoma [6, 7]. As for leiomyoma and other submucosal benign neoplasms, esophageal lipoma can benefit from minimally invasive enucleation or endoscopic resection, which are safe and effective and may reduce the potential morbidity associated with open surgery [10].
CONCLUSION
A minimally invasive approach is safe and effective in the treatment of esophageal lipoma and can be life-saving in patients with pedunculated tumors.
ACKNOWLEDGEMENTS
This work was supported by AIRES (Associazione Italiana Ricerca ESofago).
CONFLICT OF INTEREST STATEMENT
None declared.



