-
PDF
- Split View
-
Views
-
Cite
Cite
Khurum Mazhar, Aditya Narain, Saifullah Mohamed, Akshay J Patel, Qamar Abid, George Bouras, Pneumatic-aorta: an unusual aetiology for stroke, Journal of Surgical Case Reports, Volume 2020, Issue 6, June 2020, rjaa193, https://doi.org/10.1093/jscr/rjaa193
Close - Share Icon Share
Abstract
The following report describes a case in which air in the aorta led to stroke from cerebral emboli in a patient with distal oesophageal cancer. The patient presented with clinical features of a right-sided stroke. Computed tomography scans revealed air in the ascending aorta and brachiocephalic artery as a result of an oesophago-atrial fistula. The patient deteriorated and died soon after hospital admission despite conservative measures successfully dissipating the air. When encountered, emergent treatment of the underlying cause should be addressed but the outcome remains poor.
INTRODUCTION
Pneumatic aorta (pneumo-aorta) or the entrailment of air into the aorta is a very rare occurrence with either a poor prognosis or diagnosis at post-mortem. Limited case numbers have been described, the main causes being iatrogenic, such as cardiopulmonary bypass and arterial endovascular management [1]. Less well-known causes include decompression-sickness and intra-arterial gas, penetrating rib injury of the aorta and associated pneumothorax [2], transthoracic needle lung biopsy, necrotizing gastroenteritis and aorto-oesophageal fistula from chronic dissection [3]. This report describes a case of pneumo-aorta secondary to oesophago-atrial fistulation and its consequent complications.
CASE REPORT
We report a 75-year-old man with a previous diagnosis of T3N1M0 distal oesophageal adenocarcinoma, who was not considered fit enough to withstand treatment with radical intent (chemotherapy followed by surgery) due to multiple comorbidities including previous renal transplant. He was managed with palliative stenting (uncovered metal stent, Ultraflex®, Boston Scientific), and palliative radiotherapy to achieve local disease control. As per policy of the regional cancer network, there was no plan for radiological surveillance. Any imaging offered would have been expectant and after the development of new symptoms, which the patient did not have for 6 months after his treatment and up to the point of presentation.
He presented to the acute medical service with a 2-week history of increasing lethargy and dyspnoea. An initial non-contrast enhanced computed tomography (CT) scan of his chest and abdomen (Fig. 1A and B) showed a lower oesophageal perforation and migration of the oesophageal stent into the stomach. Several hours later, the patient became somnolent and examination revealed left-sided hyper-reflexia with power 0/5 (Medical Research Council scale), left-sided facial weakness and inattention. A repeat CT scan revealed air in the ascending aorta, brachiocepahlic artery and right posterior descending artery (Fig. 1C, D and E, respectively). Conservative measures were taken including nursing in the Trendelenberg position, and a repeat CT scan with contrast was organized. This third scan showed dissipation of the air, but loss of the fat plane between the left atrium and oesophagus (Fig. 1F); this was suggestive of an oesophago-atrial fistula (OAF). The patient developed seizures and his conscious level declined. He was treated with palliative intent and died a few hours later.
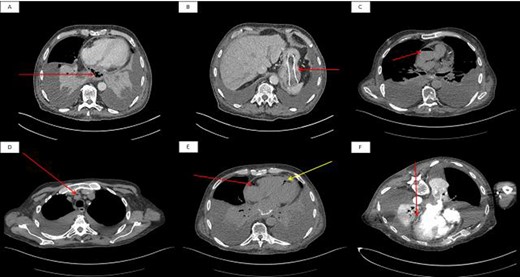
Initial non-contrast enhanced axial CT scan of the thorax. (A): The arrow shows lower oesophageal perforation with cavity containing air and debris in the posterior mediastinum. (B): The arrow shows migration of oesophageal stent into the stomach. A second non-contrast enhanced axial CT scan of the thorax showed air in the ascending aorta (C), brachiocephalic artery (D) and (E) right coronary artery (red arrow) and posterior descending artery (yellow arrow). A final contrast-enhanced axial CT scan of the thorax (prone position) shows loss of the fat plane at the junction of the oesophageal tumour and left atrium.
DISCUSSION
In the present case, an OAF caused entrailment of air into the aorta. Normal left atrial pressure is 6–12 mmHg, whereas a normal oesophageal peristaltic wave generates pressures up to 80 mmHg. While a fistula between the aorta and oesophagus would normally lead to massive gastrointestinal bleeding, fistula between the oesophagus and the lower pressure left atrium would allow passage of air into the circulation, especially upon swallowing or increased intra-thoracic pressure during coughing. Air emboli, once established in the systemic circulation, would enter the cerebral circulation and result in embolic stroke. Cerebral arterial embolism as a result of OAF has been described previously, with only one case being attributed to oesophageal carcinoma [4]. We describe the first case of pneumatic-aorta as a result of such an anomalous communication causing cerebral emboli. The proximity of the left atrial (LA) to the oesophageal wall is < 5 mm in 40% of cadaveric specimens [5]. This makes it susceptible to injury during catheter ablation for atrial fibrillation. Consequential OAF has a reported incidence of up to 1% in pulmonary vein isolation and also has a grave prognosis [6, 7]. In our case, neoplastic processes had eroded the very thin fat pad layer between the infero-posterior LA wall and distal oesophagus [5]. Fistulation introduces air, food and bacteria to the circulation resulting in sepsis and embolization to the brain with multifocal infarctions. Post-mortem reports have shown the brain to be oedematous, with variably sized haemorrhagic infarctions and smooth spaces from air emboli [3]. Treatment should be directed at reversal of the underlying cause, although, in the present case, re-stenting of the oesophagus was not possible due to the patient’s rapid deterioration. Intravenous antibiotics should be administered for sepsis from migratory oesophageal particulate matter in the systemic circulation. Pneumatic-aorta in the present case was managed by the Trendelenberg position and repeat CT scan showed resolution by this measure.
CONCLUSION
This case adds OAF to the list of aetiologies for pneumatic aorta. Furthermore, we provide evidence that simple conservative measures aid in its dissipation; it is still, unfortunately, associated with a poor outcome.
CONFLICTS OF INTEREST
None declared.
FUNDING
None.



