-
PDF
- Split View
-
Views
-
Cite
Cite
Jonathan Rogozinski, R Michael Johnson, Vascularized tendon graft to the central slip using a finger fillet flap, Journal of Surgical Case Reports, Volume 2020, Issue 6, June 2020, rjaa192, https://doi.org/10.1093/jscr/rjaa192
Close - Share Icon Share
Abstract
Burn boutonniere deformity (BBD) treatment remains a challenge in reconstructive surgery. Severe hand defects after burn/trauma may be reconstructed with nonsalvageable or amputated tissue. The fillet flap (FF) is generally used as “spare parts” in the trauma algorithm for mangled extremities. This case study examines the use of a FF with concurrent repair of the adjacent finger extensor tendon with the amputated finger flexor tendon after burn injury. The goal is to provide adequate tissue coverage using a finger FF while concurrently reconstructing the central slip of the extensor tendon with the transposed flexor tendon from an adjacent nonfunctional digit. After reconstruction, no subluxation of the extensor tendon occurred with manipulation. Despite prolonged rehabilitation due to injuries, the surgical site healed appropriately. Single-stage FF reconstruction with vascularized tendon grafts should be considered in selected patients with BBD. This novel idea can be applied to the management of traumatized extremities.
INTRODUCTION
The treatment of burn boutonniere deformity (BBD) remains a challenging issue in reconstructive surgery. Fourth degree burns with the loss of tendon structure add to the complexity of the injury and frequently lead to permanent impairment. The pathophysiology and options for improving function have been previously detailed by Groenevelt [1].
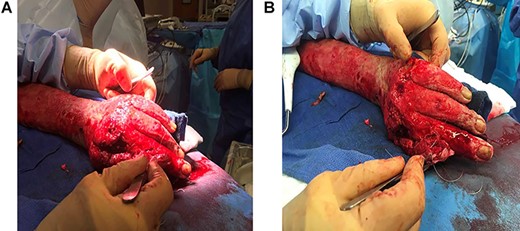
(A and B) Intraoperative photos of the index finger amputation along with the FF covering of the long finger with the salvaged.
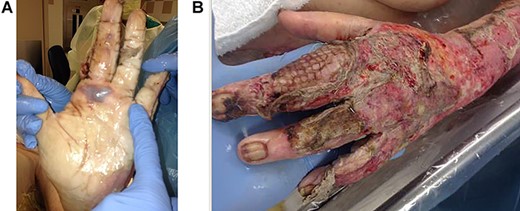
(A and B) Images of the patients’ left hand after repair using the FF technique along with the reconstruction of the central slip of the EDC and the extensor tendon of the EDC.
Multiple digits may be involved in severe injuries. If an adjacent digit is unsalvageable or severely damaged, spare parts or fillet flap (FF) surgery may be an option to improve function in the adjacent digit. The authors have found this technique useful for the coverage of extensor tendons in the past [2]. The logical extension of this technique is to restore tendon function of the tendon as well as providing skin and soft tissue coverage.
In this case report, we describe a novel way to provide adequate tissue coverage using a finger FF while concurrently reconstructing the central slip of the extensor tendon with the transposed flexor tendon from an adjacent nonfunctional digit.
CASE REPORT
A 67-year-old male with a history of chronic obstructive pulmonary disease was involved in a home oxygen explosion and suffered extensive burns to his body. He was found to have ~30.5% total body surface area burns. The burns were primarily third and fourth degree. He underwent multiple excision and grafting procedures and a left above knee amputation by the primary burn team before plastic surgery consultation.
Plastic surgery was consulted 5 weeks after the initial injury. On post burn Day 38, the patient was operated for further debridement reconstruction of the left long finger. The extent of the injury was confirmed in this procedure. It was apparent that the dorsal left hand had desiccated. The exposure of extensor tendons and joint capsule of the metacarpal phalangeal joint (MCP) and proximal interphalangeal joint (PIP) of the index finger occurred, along with the exposure of the PIP joint of the long finger. The index finger was determined to be nonfunctional; however, the volar aspect was viable, which could be used for the reconstruction of the damaged dorsal long finger.
The granulation and nonviable tissue were sharply debrided with Versajet® (Smith-Nephew, Andover, Massachusetts) (Figure 1). A small defect in the long finger soft tissue over the MCP was repaired with 3–0 chromic suture. The bones and nail matrix were excised from the index finger and the flap was then transposed on the dorsum of the long finger. The index ray metacarpal was resected in order to achieve this. The flexor digitorum profundus (FDP) tendon of index was used as a vascularized tendon graft to reconstruct the extensor tendon of the long finger as well as the central slip of the extensor digitorum communis (EDC) (Figure 2). The extensor tendon was debrided proximally to healthy tendon, and 4–0 supramid suture was used in a figure of 8 patterns for the tendon anastomosis. This was done circumferentially to replace the entire area of missing connective tissue and extensor tendon. Proximally, the FDP tendon was divided to prevent the flexor from being the driver of extension of the finger. This maneuver defines this procedure as a vascularized tendon graft as opposed to a tendon transfer. Now the primary driving force of the transferred tendon was the EDC and the lateral bands. Split thickness skin grafts were used to cover the dorsum of the hand. The patient was stable for discharge to long-term acute care (LTAC) on post burn Day 45. Patient was lost to follow up after transfer from LTAC. Unfortunately, he expired ~3 months after discharge from the LTAC and long-term follow-up was unavailable.
DISCUSSION
Concern for joint contracture and disruption of the tendon gliding environment are ever present when severe digital burns occur. The FF maintains excellent sensibility, coverage and color match, appropriating length and preventing the need for more proximal amputation [3, 4].
The results of treatment of BBD are primarily determined by the severity of the injury at presentation. Conservative treatment of mild deformities can be effective with splinting if there is adequate soft tissue coverage on the extensor surface [5]. Duzgun et al. [6] demonstrated a reduction of extension deficit from 54 to 7 degrees with nonvascularized palmaris longus tendon graft. Rico et al. [7] found that 42% of their patients had good to excellent results in patient who presented with 60 degrees of deformity nonvascularized tendon grafts. Another study of 22 patients demonstrated only 15–30 degrees of improvement with nonvascularized tendon reconstruction, indicating the need for innovative procedures in the treatment of BBD [1].
Adequate skin and soft tissue coverage is a prerequisite to improving outcomes in a severe deformity. Grishkevich demonstrated a three-stage technique in the treatment of severe BBD with 90-degree deficits and soft tissue deficits. With this technique, 62% of patients had a good to excellent outcome in this difficult subset of patients [8].
All of the previous techniques for the reconstruction of BDD utilized nonvascularized palmaris longus tendon grafts as the primary donor source. The exception is a flexor digitorum superficialis technique with a drill hole thru the middle phalanx, described by Stack in 1971 [9]. This case report is the first to demonstrate the FDP tendon as a donor source for the reconstruction of the central extensor tendon at the PIP joint with the added advantage of single-stage soft tissue coverage.
There are obvious limitations to this report. Although the concept and technical aspect of this procedure may be sound better, the patient did not survive long enough to prove the outcome to be a success. Only patients with multiple severely injured digits will be candidates for this procedure.
CONCLUSION
Burn outcomes are primarily predetermined by the extent of the injury. Single-stage FF reconstruction with vascularized tendon grafts and skin flap coverage is technically feasible and should be considered in carefully selected patients with BBD.
CONFLICT OF INTEREST STATEMENT
None declared
FUNDING
No funding was received for this work.



