-
PDF
- Split View
-
Views
-
Cite
Cite
Tim Harding, Enda Hannan, Conor Brosnan, William Duggan, David Ryan, Anthony Stafford, Donal Maguire, The dilemma of the duplicated cystic duct: a case report, Journal of Surgical Case Reports, Volume 2020, Issue 6, June 2020, rjaa161, https://doi.org/10.1093/jscr/rjaa161
Close - Share Icon Share
Abstract
We present a rare case of a duplicated cystic duct encountered during an elective laparoscopic cholecystectomy in a patient with biliary colic. Prompt recognition of an intraoperative bile leak followed by thorough examination and recognition of the source allowed for timely and appropriate management of the affected patient with a satisfactory post-operative outcome. Our case is unique by the lack of availability of intraoperative cholangiogram at the time of surgery, which posed a significant diagnostic and therapeutic challenge, and by how aberrant anatomy was confirmed intraoperatively by reviewing prior cardiac magnetic resonance imaging. Unremarkable preoperative imaging does not rule out the presence of abnormal anatomy. Early involvement of a specialist hepatobiliary surgeon is essential in an unexplained bile leak, with a low threshold in converting to an open procedure if there is difficulty in clearly deciphering anatomy.
INTRODUCTION
Laparoscopic cholecystectomy (LC) is the most common elective laparoscopic procedure performed globally and is the gold standard treatment for gallstone disease [1]. The bile duct injury (BDI) remains the most dreaded complication, with an incidence rate of 0.3% [2, 3]. Clear identification of biliary anatomy and establishing the critical view of safety is essential in avoiding BDI. However, this can be challenging, with variations in biliary anatomy in ~47% of patients [3]. An extremely rare variant is the duplicated cystic duct [4].
We report a patient found to have two cystic ducts during elective LC. Our case is unique as intraoperative cholangiogram (IOC) was not available at the time of the procedure, which posed significant diagnostic and therapeutic challenges.
CASE REPORT
A 78-year-old female underwent elective LC for treatment of biliary colic. She had no significant medical history apart from previously investigated atypical chest pain. A gallbladder ultrasound showed multiple gallstones and a normal common bile duct. Her liver function tests (LFTs) were unremarkable. The procedure commenced as a standard four-trocar LC. Once the critical view of safety was established, the cystic duct and cystic artery were secured by clips and divided.
Dissection of the gallbladder from the liver commenced with electrocautery. A small bile leak became evident within the gallbladder fossa. This appeared to correspond with a small hole in the gallbladder. However, with further separation of the gallbladder from the liver, it became evident that the source of bile was from an open tubular structure in the gallbladder fossa. To allow for adequate evaluation of this bile leak, the decision was made to convert to an open procedure. Two consultant hepatobiliary surgeons attended to offer further assistance.
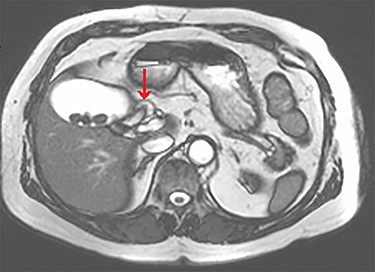
The tubular structure was remote from the porta hepatis with one lumen. It was located within the distal gallbladder fossa. Inspection of the gallbladder demonstrated an opening at the same orientation and of the same calibre as this tubular structure, raising suspicion for a duplicated cystic duct. Probing the source of the bile leak confirmed a single lumen. The capacity to perform IOC was not available at the time of the operation. A review of the patient’s prior imaging was performed. Recent cardiac magnetic resonance imaging (MRI), while not dedicated magnetic resonance cholangiopancreatography (MRCP), provided adequate views of the liver, gallbladder and biliary tree to demonstrate the suspected anomaly. On these images, two structures were seen to be connecting the gallbladder to the biliary tree. One duct was observed at Hartmann’s pouch, while a second connected to the gallbladder body (Fig. 1, Fig. 2). The images confirmed suspicion of a duplicated cystic duct and the decision was made to clip the lumen. The cholecystectomy was completed and a drain placed in the gallbladder fossa.

Axial view of the liver and gallbladder from a cardiac MRI showing a tubular structure entering the gallbladder at the level of the body in keeping with an accessory cystic duct (highlighted by the arrow).
Axial view of the liver and gallbladder from a cardiac MRI showing the normal location of the cystic duct entering Hartmann’s pouch (highlighted by the arrow), which is separate and distinct from the structure shown in figure 1.
The patient had a subsequently uneventful post-operative course. Her MRI images were reviewed in the post-operative period by two senior radiologists who concurred that the view of the liver on the cardiac MRI demonstrated two separate cystic ducts. Given that she remained clinically well with normal LFTs, no bilious output in the drain and that her prior imaging had adequately demonstrated the anomaly according to two senior radiologists, no further imaging was performed. She was discharged home 5 days post-operatively and remains well at outpatient follow-up with persistently normal LFTs. Her final histology showed evidence of chronic cholecystitis with cholelithiasis.
DISCUSSION
With more than half a million cholecystectomies performed annually, variations in biliary anatomy present a significant challenge for laparoscopic surgeons. Duplication of the cystic duct is extremely rare, with only 20 previous cases reported in the literature [4]. Three types of duplicated cystic ducts have been previously described: The ‘Y’ type, in which two cystic ducts meet to form a common channel, the ‘H’ type, in which the accessory duct enters into the right, left or common hepatic duct and the trabecular type, in which the accessory duct enters the liver substance directly [3,4].
Our case represents a form of the ‘H’ type, with imaging and intraoperative evaluation suggesting that the accessory duct entered the left hepatic duct. Our case is unique by the lack of availability of IOC, which posed a challenge in establishing the source of bile leak. This is not an unusual scenario for laparoscopic surgeons to potentially find themselves in, with routine IOC not being widely available and may not always be possible in many centres performing elective LC [5]. However, by thorough inspection of the specimen and source of the leak, review of available imaging and involvement of specialist hepatobiliary surgeons, there was significant evidence to suggest that this represented an accessory cystic duct, allowing for safe completion of the procedure in the absence of IOC.
While preoperative MRCP or endoscopic retrograde cholangiopancreatography (ERCP) may identify abnormal anatomy, this is not guaranteed to prevent encountering unexpected variations. Of the seven reported cases of cystic duct duplication where a preoperative ERCP was performed, only three had the anomaly detected [4]. In most cases, the second cystic duct was an intraoperative finding [4]. This emphasizes the importance of constant vigilance during LC even when preoperative imaging yields no abnormality.
Our case highlights numerous important points for performing safe LC with abnormal biliary anatomy. Early involvement of a specialist hepatobiliary surgeon is essential with a suspected biliary injury or unexplained bile leak, especially if IOC is unavailable. When anatomy cannot be deciphered, one should have a low threshold for conversion to laparotomy. Close observation in the post-operative period is also critical. Even if it is felt that the bile leak has been successfully dealt with at the time of surgery, a drain should be placed to ensure no ongoing bile leak. If an ongoing leak is suspected, this should be promptly evaluated by MRCP or ERCP.
In conclusion, the duplicated cystic duct is a highly uncommon variant of biliary anatomy, which may pose a significant dilemma to the laparoscopic surgeon. Constant vigilance for anatomical variance is essential to avoid adverse outcomes, with early involvement of a hepatobiliary specialist if there is unexplained bile leakage. Unremarkable preoperative imaging does not exclude the presence of abnormal anatomy.
FUNDING
No funding received.
CONFLICT OF INTEREST
None declared.



