-
PDF
- Split View
-
Views
-
Cite
Cite
Shigeo Ninomiya, Syunsuke Fujita, Tadashi Ogawa, Yoshitake Ueda, Norio Shiraishi, Masafumi Inomata, Katsuhiro Shimoda, Incarcerated femoral hernia treated with elective totally extraperitoneal repair: a case report, Journal of Surgical Case Reports, Volume 2020, Issue 6, June 2020, rjaa158, https://doi.org/10.1093/jscr/rjaa158
Close - Share Icon Share
Abstract
Incarcerated groin hernia is a common surgical emergency. However, reports of incarcerated femoral hernia treated with elective totally extraperitoneal repair are extremely rare. A 62-year-old woman visited our hospital with lower abdominal pain and bulging from a right groin lesion. The patient was diagnosed as having right incarcerated femoral hernia containing greater omentum by computed tomography. As there were no clear findings of intestinal obstruction and peritonitis, elective surgery was performed. Intraoperatively, the hernia sac had herniated into the right femoral canal. We could release the hernia sac using laparoscopic forceps. After reduction of the hernia sac, polypropylene mesh was placed in the preperitoneal space and fixed to Cooper’s ligament. The patient’s postoperative course was uneventful, and she was discharged 3 days after surgery. We consider elective totally extraperitoneal repair for incarcerated femoral hernia to be an effective procedure for selected patients who have been diagnosed accurately.
INTRODUCTION
Incarcerated groin hernia, defined as the inability to reduce the hernia content from the abdominal wall, is a common surgical emergency that accounts for 5–15% of abdominal hernias. Femoral hernias are relatively rare, accounting for 3–4% of all groin hernias [1]. Also, they frequently present with incarceration, resulting in small bowel obstruction and strangulation. Kim et al. [2] reported that about 35–43% of femoral hernias caused a surgical emergency with high rates of laparotomy and bowel resection. Therefore, accurate diagnosis and early surgical treatment are important in treating patients with femoral hernia.
With the advances in endoscopic surgery, the number of endoscopic surgeries for groin hernia has gradually increased. According to a national survey in Japan [3], endoscopic procedures were performed in 87 327 patients from 1990 to 2017: 64 195 (73.5%) underwent transabdominal preperitoneal (TAPP) repair, and 23 131 (26.5%) underwent total extraperitoneal (TEP) repair. However, reports of incarcerated femoral hernias treated with elective TEP repair are extremely rare. We report a case of incarcerated femoral hernia containing greater omentum that was treated with elective TEP repair.
CASE REPORT
A 62-year-old woman visited our hospital with a 1-day history of lower abdominal pain and bulging from a right groin lesion. Her physical examination showed a right inguinal bulge and pain. Her abdomen was not distended and was without rebound tenderness and muscular defense. However, the bulge in the right groin lesion could not be reduced manually. Contrast-enhanced computed tomography showed a hypodense rounded lesion medial to the right femoral vessels (Fig. 1A) with fluid collection (Fig. 1B), with no intestinal obstruction or ischemia. Based on these physical and radiological findings, the patient was diagnosed as having a right incarcerated femoral hernia containing fat tissue. As there were no clear findings of intestinal obstruction, elective TEP repair was performed 1 day after admission following preoperative evaluation of her general condition. An infra-umbilical incision was made under general anesthesia. The preperitoneal space was created with blunt dissection with the aid of CO2 gas insufflation to a pressure of 12 mmHg. Two 5-mm trocars were inserted into the left mid-abdomen. The hernia sac had herniated into the right femoral canal (Fig. 2A). Therefore, we diagnosed a right incarcerated femoral hernia containing greater omentum. However, there were no findings of abscess formation or small bowel necrosis. We were able to release the hernia sac using laparoscopic forceps (Fig. 2B). After reduction of the hernia sac, 10.3 × 15.7 cm polypropylene mesh was placed in the preperitoneal space and fixed to Cooper’s ligament with a fixation device (ProTack™, COVIDIEN) (Fig. 3). Intraperitoneal observation was not performed because we considered it unnecessary to confirm the presence of intestinal damage. The patient’s postoperative course was uneventful, and she was discharged from our hospital 3 days after surgery. Presently, at 1 month after surgery, the patient is doing well without recurrence or mesh infection.
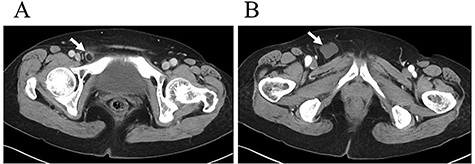
Contrast-enhanced computed tomography showed a hypodense rounded lesion (A, arrow) medial to the right femoral vessels with fluid collection (B, arrow).
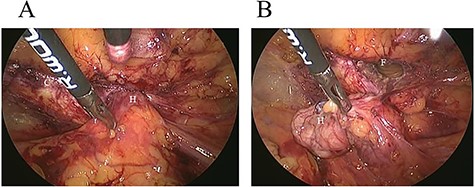
Intraoperative findings. A: The hernia sac (H) had herniated into the right femoral canal. B: The hernia sac (H) was released from the femoral canal (F) with laparoscopic forceps.
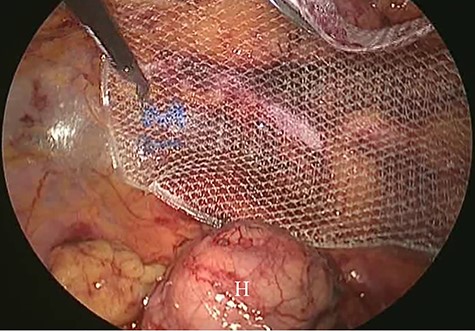
Intraoperative findings (2). Polypropylene mesh was placed in the preperitoneal space. Hernia sac (H).
DISCUSSION
Although our patient was diagnosed as having a right incarcerated femoral hernia, the hernia content was considered to be greater omentum based on contrast-enhanced computed tomography findings. Also, there were no findings of intestinal obstruction and peritonitis. Therefore, we performed elective surgery after evaluation of her general condition. In general, there are higher rates of postoperative complications and mortality with emergency surgery than with elective surgery [4]. Especially, it has been reported that the incidence of postoperative complications in conventional emergency repair of incarcerated groin hernia ranges from 21 to 39%, with a mortality rate of 4–5% [5, 6]. To our knowledge, our case is the first report of initially elective TEP repair under an accurate diagnosis of incarcerated femoral hernia containing greater omentum. It is important to obtain an accurate diagnosis to avoid unnecessary emergency surgery.
Open conventional hernia repairs such as Lichtenstein hernioplasty are not effective for the treatment of femoral hernias. Therefore, endoscopic surgery is recommended for their treatment. However, it is controversial which is better for the treatment of incarcerated femoral hernia, TEP or TAPP repair. According to the above-mentioned national survey in Japan, the number of TAPP repairs was greater than that of TEP repair (73.5 vs. 26.5%, respectively) [3]. In TAPP repair, intraperitoneal observation can aid in diagnosing the viability of the hernia content. In addition, resection of the hernia content can be carried out via a small laparotomy if necessary [2]. However, the European Hernia Society guidelines recommend TEP repair for the treatment of groin hernia with low risk of injury to the other intraperitoneal organs [7]. We selected TEP repair in our case because intraperitoneal observation was not necessary based on the preoperative diagnosis. Sasaki et al. [8] reported two-stage laparoscopic treatment with TEP repair followed by intestinal resection assisted by intraperitoneal laparoscopic exploration. Kim et al. [2] also reported TEP repair followed by a diagnostic laparoscopy. To our best knowledge, only four cases of incarcerated femoral hernia treated with TEP repair have been reported to date (Table 1) [2, 8, 9]. It is important to use TEP or TAPP repair properly based on the individual case.
Reported cases of incarcerated femoral hernia treated with totally extraperitoneal repair (including our case)
| Authors . | No. of cases . | Elective/emergency . | Remarks . |
|---|---|---|---|
| Sasaki et al. [8] | 2 | Elective (two-stage) | Followed by intestinal resection (two-stage) |
| Kim et al. [2] | 1 | Emergency | Followed by diagnostic laparoscopy |
| Namba et al. [9] | 1 | Emergency | Single-port totally extraperitoneal repair |
| Our case | 1 | Elective | Initial elective surgery |
| Authors . | No. of cases . | Elective/emergency . | Remarks . |
|---|---|---|---|
| Sasaki et al. [8] | 2 | Elective (two-stage) | Followed by intestinal resection (two-stage) |
| Kim et al. [2] | 1 | Emergency | Followed by diagnostic laparoscopy |
| Namba et al. [9] | 1 | Emergency | Single-port totally extraperitoneal repair |
| Our case | 1 | Elective | Initial elective surgery |
Reported cases of incarcerated femoral hernia treated with totally extraperitoneal repair (including our case)
| Authors . | No. of cases . | Elective/emergency . | Remarks . |
|---|---|---|---|
| Sasaki et al. [8] | 2 | Elective (two-stage) | Followed by intestinal resection (two-stage) |
| Kim et al. [2] | 1 | Emergency | Followed by diagnostic laparoscopy |
| Namba et al. [9] | 1 | Emergency | Single-port totally extraperitoneal repair |
| Our case | 1 | Elective | Initial elective surgery |
| Authors . | No. of cases . | Elective/emergency . | Remarks . |
|---|---|---|---|
| Sasaki et al. [8] | 2 | Elective (two-stage) | Followed by intestinal resection (two-stage) |
| Kim et al. [2] | 1 | Emergency | Followed by diagnostic laparoscopy |
| Namba et al. [9] | 1 | Emergency | Single-port totally extraperitoneal repair |
| Our case | 1 | Elective | Initial elective surgery |
The use of polypropylene mesh for incarcerated groin hernia also remains controversial. Several recent retrospective studies have shown that the use of mesh can be safe and effective in patients with an incarcerated groin hernia and that it reduced the recurrence but did not increase the opportunity for mesh infection [5, 6]. Dai et al. [10] reported that the use of mesh did not increase the infection rate in their cohort study. We considered the use of mesh to be acceptable in our case because there was no bowel obstruction or necrosis. Also, we considered it unnecessary to insert a drainage tube into the peritoneal cavity. Further accumulation of cases and randomized controlled trials are needed to determine whether the use of mesh is safe and effective in the treatment of incarcerated groin hernias.
In conclusion, we consider elective TEP repair for incarcerated femoral hernia to be an effective procedure for selected patients who have been diagnosed accurately.
Conflict of Interest Statement
The authors have no conflict of interest to declare.



