-
PDF
- Split View
-
Views
-
Cite
Cite
Shin Ueda, Keisuke Okada, Maki Kanzawa, Teruo Fukuda, Junya Furukawa, Masato Fujisawa, A case of prostate stromal sarcoma involving the rectum, Journal of Surgical Case Reports, Volume 2020, Issue 6, June 2020, rjaa165, https://doi.org/10.1093/jscr/rjaa165
Close - Share Icon Share
Abstract
Sarcomas and related proliferative lesions of the specialized stroma of the prostate are very rare and have been classified into prostate stromal sarcoma (PSS) and prostatic stromal tumor of uncertain malignant potential based on histology. We herein describe a case of PSS. A 40-year-old male presented at a hospital with urinary distention. Magnetic resonance imaging revealed a large prostate mass, and the diagnosis was prostate sarcoma of uncertain differentiation by ultrasound-guided needle biopsy. Total pelvic exenteration was performed and a pathological diagnosis of PSS was ultimately reached. Ten months later, there have been no signs of metastasis or recurrence.
INTRODUCTION
Gaudin et al. classified sarcomas and related lesions of the specialized prostatic stroma [1]. These prostatic stromal tumors originate from mesenchymal components of the prostate and are grouped into two clinicopathological categories: prostate stromal sarcoma (PSS) and prostatic stromal tumor of uncertain malignant potential (STUMP). PSS is a rare prostate sarcoma and the most common symptom is urinary retention [2].
We herein report a case of PSS in a 40-year-old man who presented with urinary retention.
CASE REPORT
A 40-year-old man presented at a local hospital with urinary distention and was catheterized. Ultrasonography revealed a large prostatic mass; however, his prostate specific antigen (PSA) level was 0.62 ng/ml, which was within the normal range (<4.0 ng/ml). He was referred to our hospital for further examination and treatment. The patient had no pain, fever or abdominal distension. The results of a physical examination were normal and all other blood routine indexes were within normal limits. Other tumor markers, including CEA, CA19–9, CA-125, SCC and CYFRA, were also within normal limits. A digital rectal examination confirmed that the prostate was enlarged with perceptible nodules and a less clear border. Pelvic transabdominal ultrasound revealed an enlarged heterogeneous prostate mass. Magnetic resonance imaging (MRI) showed an enlarged, heterogeneous mass of 5.5 cm in the right prostate lobe (Fig. 1A and B). Vesical invasion was suspected by cystoscopy (Fig. 1C). In addition, positron emission tomography–computerized tomography and colonoscopy revealed rectal invasion of the tumor (Fig. 1D).
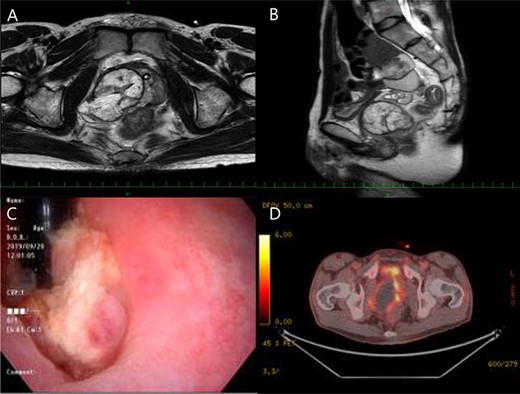
Magnetic resonance imaging (MRI) showed an enlarged, heterogeneous mass of 5.5 cm in the right prostate lobe (A, B), and vesical invasion was suspected by cystoscopy (C), besides positron emission tomography-computerized tomography and colonoscopy revealed rectal invasion of the tumor (D).
Based on his symptoms and the results of examinations, a provisional diagnosis of prostatic sarcoma was considered. We performed transrectal needle biopsy of the tumor. The pathological result was PSS or prostatic STUMP.
Bladder and rectal invasion by the tumor was detected, whereas the invasion of other adjacent organs and enlarged lymph nodes were not observed. Total pelvic exenteration was performed with tubeless ureterostomy. An incision was made in the middle of the lower abdomen with transanal minimally invasive surgery.
Macroscopically, a 55 × 55 × 50-mm soft solid tumor with necrosis and a bleeding smooth surface was visible in the prostate (Fig. 2A). There was no obvious adhesion between the tumor and bladder.
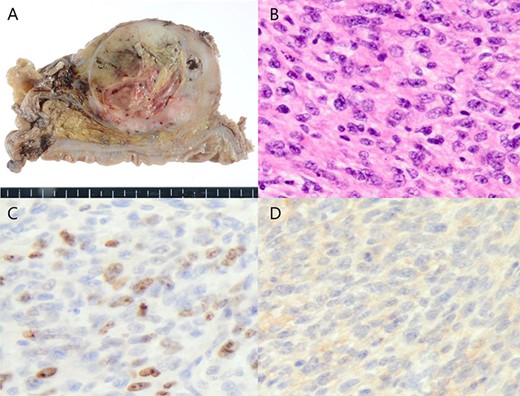
Macrospically, a 55 × 55 × 50-mm soft solid tumor with necrosis and a bleeding smooth surface was visible in the prostate (A), microscopically, the tumor was growing with invasive potential (B), and immunohistochemical results showed that CD34 were slightly positive (C), besides the Ki-67 labeling index was 20% (D).
Microscopically, the tumor was growing with invasive potential (Fig. 2B). It spread into the seminal vesicles and invaded the rectal muscularis propria. There was no tumor invasion of the bladder, and the surgical margin was cancer-negative. According to the examinations, gastrointestinal stromal tumor or solitary fibrous tumor was listed as differential disease. However, c-kit was negative and stat 6 was also negative, so both were denied. The Ki-67 labeling index was 20% (Fig. 2C). Immunohistochemical results showed that vimentin and CD34 were positive (Fig. 2D), whereas PSA was negative. The final diagnosis of PSS was reached based on histopathological results.
The retropubic drainage tube was removed 2 days after surgery and the bilateral ureter catheter 7 days after surgery. The patient was discharged from the hospital 10 days after surgery with no complications. The patient received four courses of adjuvant chemotherapy with doxorubicin and ifosfamide, and there has been no evidence of recurrence for >10 months after surgery.
DISCUSSION
Prostate sarcoma is a very rare malignancy with a poor prognosis. It originates from the mesoderm in the reproductive tract. Risk factors are considered to be a previous history of prostatitis, perineal trauma, previous prostate biopsy and radiation; however, the present case had none of these risk factors. The main subtypes of prostate sarcoma are rhabdomyosarcoma and leiomyosarcoma. PSS and STUMP are rare among prostate sarcoma and are classified as unclassified sarcoma.
To the best of our knowledge, the first PSS case report was published in 1998, and only ~30 cases have since been reported [1–3]. The age of patients with PSS ranges between 30 and 40 years, which is younger than that of prostate cancer patients. Although the majority of PSS patients have dysuria, urinary retention and hematuria, there are no specific clinical symptoms of PSS. Therefore, the tumor is not detected until the prostate mass becomes large and the patient is in a serious condition. Early metastases are not rare in PSS patients, with the most common metastatic site being the lungs.
In immunohistochemical studies, PSS is typically positive for vimentin, CD34 and progesterone receptors, but not estrogen receptors, which was observed in the present case. However, some cases were negative for CD34 in the literature; therefore, although immunohistochemistry is crucial for diagnosing PSS, it cannot be the sole diagnostic criterion. Furthermore, a significant increase in the Ki-67 labeling index was reported in most cases, and was 20% in the present case.
Surgical resection remains the mainstay treatment of PSS, including radical prostatectomy, cystoprostatectomy and total pelvic exenteration. It currently remains unclear whether adjuvant radiotherapy and chemotherapy prolong survival. Lam et al. [4] reported the efficacy of chemotherapy with doxorubicin and ifosfamide for lung metastasis found after radical prostatectomy and adjuvant irradiation; their patient remained free of disease for 5 months after chemotherapy and surgical resection. Sakura et al. [5] demonstrated the efficacy of chemotherapy with VP-16, ifosfamide and cisplatin (VIP) chemotherapy (VP-16 100 mg/m2, ifosfamide 1200 mg/m2 and cisplatin 20 mg/m2) for lymph node metastasis detected 5 months after radical prostatectomy; their patient remained free of disease for 4 years after treatment.
In the present case, we selected doxorubicin and ifosfamide as adjuvant chemotherapy even though neither recurrence nor metastasis was detected after surgery. The patient received four courses of chemotherapy, and there has been no evidence of recurrence for >10 months after surgery.
CONCLUSION
PSS is a rare and highly malignant tumor. When an adult male develops urinary distention and has the same MRI findings as those described above, PSS needs to be considered.
CONFLICT OF INTEREST STATEMENT
The authors declare that there are no conflicts of interests.
Funding
No funding was received for this article.



