-
PDF
- Split View
-
Views
-
Cite
Cite
Miguel A Moyon C, Gabriel A Molina, S Alexandra Valencia, Veronica M Basantes, R Alejandro Mecias, Ruben Parra, Diego R Yunga, Splenic abscess after arterial embolization: a rare cause of acute abdomen, Journal of Surgical Case Reports, Volume 2020, Issue 6, June 2020, rjaa146, https://doi.org/10.1093/jscr/rjaa146
Close - Share Icon Share
Abstract
Splenic abscess is a rare disease and a diagnostic challenge for the medical team. Attributable to its high mortality, prompt diagnosis and treatment are essential. A high degree of clinical awareness is required in conjunction with aggressive treatment, as misleading symptoms may delay treatment and worsen the patient’s prognosis. The management of splenic abscess is based on medical therapy, antibiotics and splenectomy or percutaneous drainage. We present the case of a 58-year-old patient presented with a splenic abscess after arterial embolization. He underwent surgery and completely recovered.
INTRODUCTION
Splenic abscess is an uncommon disease (0.2–0.7%) that generally occurs in patients with immunodeficiency. The incidence of this rare disease is thought to be increasing because of the rising number of immunocompromised patients (Cancer and human immunodeficiency virus) and the extensive use of imaging modalities. Symptoms are usually subtle or non-specific potentially delaying diagnosis and increasing the risk of complications in these patients. A multidisciplinary approach is essential to increase the outcome in these critical patients. We present the case of a 58-year-old patient with a splenic abscess, after prompt treatment and surgery he underwent full recovery.
CASE REPORT
Patient is a 58-year-old male, with past medical history of pancreatogenic diabetes and cholecystectomy. He presented to the emergency room with a 2-day history of severe episodes of bright red blood stool, abdominal pain and difficulty breathing. Initial evaluation revealed a dehydrated, tachycardic, hypotensive and confused patient. Complete blood count revealed severe anemia (Hb 6.5 mg/dl), lactate was 5 mmol/L, bicarbonate was 12 meq/L and creatinine level was 3.5 mg/dl. Liver chemistries were mildly elevated and the coagulation profile was normal. He was admitted to the intensive care unit (ICU), and treated with vigorous volume resuscitation, transfused 4 units of blood and vasopressors. Colonoscopy was needed nonetheless it was inconclusive as the bleeding site could not be recognized. With these findings, an enhanced abdominal computed tomography (CT) was requested revealing a 10 × 11 mm aneurysm of the left colic artery. Angiography was performed and a transcatheter arterial embolization successfully controlled the bleeding. The patient improved, vasopressors were phased out and he was discharged without any apparent complications (Fig. 1).

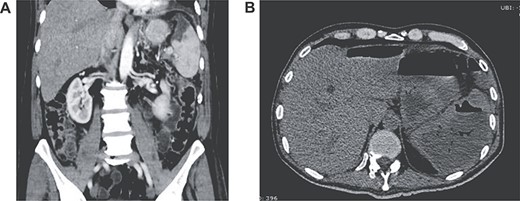
(A) Contrast-enhanced CT showing splenic infarction with inflammatory changes; (B) CT showing free liquid with a hypodense lesion.
Two weeks after discharge, he developed a high fever and acute abdominal pain in his upper left abdomen. Diffuse abdominal tenderness was detected and complementary exams revealed leukocytosis, neutrophilia, elevated C-reactive protein and increased levels of serum procalcitonin. Attributable to his background, a contrast-enhanced abdominal CT was requested detecting an enlarged spleen with a hypodense low-density lesion filled with gas. Free liquid was detected in the abdomen as well (Fig. 2A and B).
With these findings, surgery was decided. At laparotomy, 1000 cc of purulent fluid was discovered in his abdomen, the upper part of the spleen was filled with necrosis and purulent discharge. After an extensive lavage of the peritoneal cavity, a splenectomy was completed. A drain was left in place and the procedure was completed without complications. He was readmitted to the ICU for postoperative care. Escherichia coli was identified in the peritoneal liquid and after a 10-day scheme of carbapenems, he completely recovered. Pathology reported extensive necrosis of the splenic tissue; spleen abscess was the final diagnosis (Fig. 3A and B). His postoperative course was uneventful, he was discharged after full diet was initiated and the drain was removed because of low and serous output. On follow-ups, the patient is doing well.
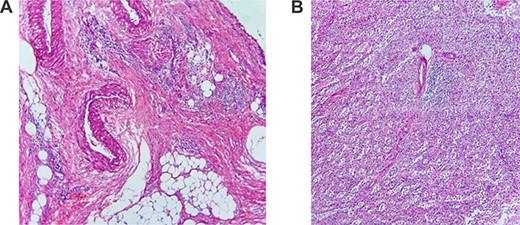
(A) Pathology of the spleen with heavy inflammatory infiltrate; (B) pathology of the spleen with necrosis.
DISCUSSION
Splenic abscess is a rare (0.2–0.7%) and potentially lethal disease [1, 2]. There has been a rise in the incidence of this condition for two main reasons, the advances of imaging studies and a greater number of patients who are immunocompromised [1, 3]. Splenic abscesses can be caused by bacteria, fungus or Mycobacterium tuberculosis [4]. Pyogenic abscesses are usually caused by Gram-negative bacteria including Staphylococcus, Streptococcus, E. coli or Salmonella. Anaerobic bacteria and Gram-positive bacteria have also been detected [1, 3, 5], as it was found in our patient.
Bacteria can reach the spleen through direct extension from a nearby infectious process, arterial embolic process, abdominal trauma, among others [1, 2]. We believe that in our case, the abscess could have been caused by the previous arterial embolization.
Clinical symptoms are non-specific and include fever, abdominal pain, weight loss and asthenia [1, 4]. Sarr and Zuidena in 1974 described the triad of fever, left upper quadrant pain and a tender mass, unfortunately, its occurrence is very rare [1, 6, 7, 11]. As these symptoms are vague, misdiagnosis and delays in therapy can potentially lead to sepsis and death [1, 7]. In our case, the patient presented with abdominal pain and fever.
Imaging studies are needed to confirm the diagnosis, ultrasonography can help, nevertheless, CT and magnetic resonance imaging provide more useful details about the abscess [8]. Pyogenic abscesses are usually a hypodense lesion ranging from 20 to 40 HU and exhibit an enhancement on the outside-facing portion of the abscesses’ wall [1, 5]. They are often unilocular but can be multifocal in ~26% of cases [1, 8]. Fungal abscesses are mostly multifocal and smaller than pyogenic, this is why these abscesses can be difficult to detect on CT [8]. Tuberculous abscesses of the spleen are seen in patients with severe, disseminated tuberculous disease. They are usually small (<2 cm), ill-defined and can show mild contrast enhancement [8, 9]. In our case, the abscess was discovered through CT.
Treatment is based on antibiotics and drainage, although, there are many reports in which percutaneous drainage can be used in some patients with good results (67–100%), splenectomy is considered the standard treatment for these patients. As these patients are regularly in critical condition mortality can be high (12.4–27.6%) [1, 10]. In our case, as the patient was in severe condition, surgery was completed and after a course of intravenous antibiotics, the patient recovered.
Diagnosis of a splenic abscess requires a high degree of suspicion since it is rarely observed and can be easily overlooked. The prognosis of the patients will depend on a timely diagnosis and on whether the infection can be controlled. We must emphasize that without adequate treatment mortality is very high; therefore, the combined teamwork of the emergency department, radiologists, surgeons and critical care physicians is vital to enhance the patient’s outcome in these rare scenarios.
Funding
None.
CONFLICT OF INTEREST STATEMENT
The authors declare no conflict of interest.
REFERENCES
Author notes
Chief of surgeon.
Attending surgeon.



