-
PDF
- Split View
-
Views
-
Cite
Cite
Yao C Huang, Elizabeth Vujcich, Jason Brown, Rare case of adhesive large bowel obstruction in acute burn patient: management of open abdomen with ABTHERA ADVANCE™ Open Abdomen Dressing, Journal of Surgical Case Reports, Volume 2020, Issue 6, June 2020, rjaa129, https://doi.org/10.1093/jscr/rjaa129
Close - Share Icon Share
Abstract
Large bowel obstructions (LBO) are rarely caused by adhesions. Surgical management of this condition may require an open approach but closure may not always be possible. There are many temporizing measures in clinical use; however, the ABTHERA ADVANCE™ Open Abdomen Dressing has demonstrated significantly improved outcomes compared to other negative pressure wound therapy dressings. There are few cases in the literature documenting adhesive LBO and none in an acutely unwell burn patient whose abdomen subsequently required the ABTHERA ADVANCE™ Open Abdomen Dressing. We emphasize the importance of considering adhesive LBO as a differential in bowel obstruction and highlight a novel but effective way of managing it in our unique case.
INTRODUCTION
Large bowel obstructions (LBO) are often due to neoplasms or caecal and sigmoid volvuli [1–3]. Other causes include diverticular disease, inflammatory bowel disease, faecal impaction or herniation [1]. Though adhesions and hernias alone contribute to 42.3% of bowel obstructions, adhesions are almost universally associated with small bowel obstructions [3]. There are few reported cases of adhesive LBO and only a single case secondary to previous appendicectomy [2]. Management may include laparotomy.
Laparotomy closure can be complicated by bowel oedema or abdominal wall tension, which risks wound dehiscence or abdominal compartment syndrome especially in patients with severe burns [4, 5]. Additionally, abdomens may be left open with intention for planned ‘re-look’ to ensure bowel viability [5]. Open abdomens are associated with increased risk for enterocutaneous fistulas, abdominal wall retraction, ventral defects and herniation and bacterial colonization [4]. As such, temporizing closure is utilized which include skin-only closure, loose packing of open fascial defects, silos or more recently, negative pressure wound therapy (NPWT) [5]. One such new NPWT is the ABTHERA ADVANCE™ Open Abdomen Dressing.
CASE REPORT
An intubated 53-year-old man was transferred to a tertiary burn centre with 24% total body surface area (TBSA) burns to the head, back, arms, legs and inhalation injury secondary to a caravan explosion. Medical history included chronic alcoholism, active smoker and a previous open appendicectomy. Despite fluid resuscitation as per Parkland’s formula, inotropic support was still required. Computer tomographic (CT) trauma series demonstrated stable old and new cervical, thoracic and sacral fractures. He was admitted to the intensive care unit for continued resuscitation.
By day five of admission all burns, including full thickness burns on his back and arms, were debrided and grafted with no further coverage required. On day nine, he developed paralytic ileus, which required colonoscopic decompression. Colonoscopy showed faecal impaction and large, coalescent ulcers in the sigmoid colon suggestive of stercoral colitis.
Subsequently, he remained stable in his systemic inflammatory state tachycardic to 115, blood pressure of 114/59 with minimal noradrenaline requirement, and febrile to 39°C. He had continued small liquid stools and developed larger nasogastric aspirates. Abdomen was tense, distended and tender on the right lower quadrant. He was not peritonitic and bowel sounds were not appreciable. Repeat imaging demonstrated a thickened caecal wall, pericaecal fat stranding and a transition point in the ascending colon secondary suspected stercolith (Fig. 1).

CT demonstrated a thickened caecal wall with pericaecal fat stranding; gastrografin had only passed through small bowel with a transition point identified in his ascending colon secondary to a suspected stercolith.
Due to failure of medical management and a mechanical obstruction, the patient received an emergency laparotomy. The greater omentum off the hepatic flexure was found to be adhered to the right iliac fossa at the previous open appendicectomy site causing flexion narrowing of the ascending colon. This was released with diathermy ablation. Multiple segments of viable small bowel appeared oedematous with venous congestion. No bowel resection was performed however 1.3 L of fluid was suctioned from the peritoneal cavity and 1.2 L aspirated from the nasogastric tube. Given the distended loops of bowel, tight abdominal wall, and plan for relook, temporary abdominal closure was achieved with ABTHERA ADVANCE™ Open Abdomen Dressing (Fig. 2).
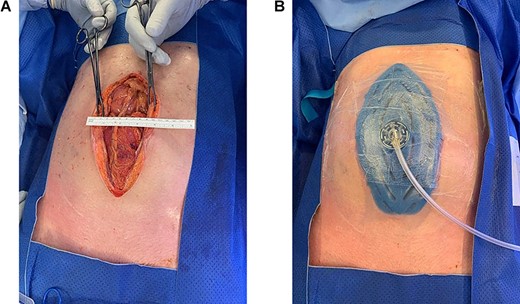
Given the distended loops of bowel, tight abdominal wall and loss of domain, and plan for relook, the decision was made for temporary abdominal closure with the ABTHERA ADVANCE™ Open Abdomen Dressing.
Relook 24 h later, demonstrated viable bowel and abdomen closure was achieved. Total parental nutrition was subsequently weaned over the week. Extubation and discharge to the ward occurred 2 weeks after presentation. His recovery was complicated by a hospital-acquired pneumonia and large pleural effusion, which was managed with antibiotics and a chest drain. He was discharged to rehabilitation 7 weeks from presentation.
DISCUSSION
Only a handful of studies describe adhesive LBO and of these; one case was secondary to appendicectomy adhesions [2]. There are no cases of adhesive LBO occurring in the critically unwell intubated burn patient, requiring a temporizing open abdomen dressing.
The most common cause of LBO in adults is neoplasms [6]. Adhesive LBO is a rare phenomenon and when present is often secondary to congenital bands, epiploic appendages, post-operative adhesions, primarily gynaecological or abdominal inflammatory causes [2, 6]. It is suggested that the involved segment of colon is usually redundant thus acting similarly to small bowel [1].
There are no systematic literature reviews on the outcomes or management of adhesive LBO. Individual studies have managed these cases with laparotomy, division of adhesive bands and resection of any ischaemic bowel [1, 2, 6]. A similar approach was utilized in this case. However, due to dilated loops of small bowel, risk of raised intraabdominal pressure, and difficulty in closure, the ABTHERA ADVANCE™ Open Abdomen Dressing was placed as a temporary dressing. Though a laparoscopic approach may have avoided this, there is a 10% associated increased incidence of bowel intervention required, with conversion to open occurring in a third of cases [7]. Improved morbidity was observed if the surgery was performed open or had an early conversion to open [7].
Abdominal compartment syndrome may be an indication for laparotomy in burn patients. Raised abdominal pressure can be present in up to 70% of major burn patients and is thought to be largely related to large volume fluid resuscitation [4]. Risk factors include a >60% TBSA burns, concurrent inhalation injury or abdominal injury—carrying a 75% mortality rate [4]. These abdomens almost always require temporizing dressings as definitive closure is generally unfeasible due to the high rate of fascial dehiscence even in instances of purported ‘tension-free’ closure [5]. This was only successful in 26% of cases despite NPWT [5].
ABTHERA ADVANCE™ Open Abdomen Dressing was utilized in our case as a temporizing measure pending return to theatre allowing relook and tension-free closure. Compared to traditional vacuum dressings, this novel dressing significantly improves wound fluid evacuation, wound contracture without a significant reduction of blood flow and reduces fascial retraction [8]. Additionally, this dressing can be placed directly over sensitive structures, such as intestines, vascular grafts, flaps and exposed pericardium [9]. As such, this demonstrates the versatility and effectiveness of the new ABTHERA ADVANCE™ Open Abdomen Dressing.
In conclusion, adhesive LBO is rare but potential cause for the obstructed patient. Though its management and post-operative care in an acutely unwell burn patient may be challenging, the ABTHERA ADVANCE™ Open Abdomen Dressing provides a safe and effective means of temporizing the abdomen pending relook and definitive closure with excellent outcomes.
CONFLICT OF INTEREST
The publication of this article has been funded by Acelity L.P.Inc.
ACKNOWLEDGEMENTS
None.
REFERENCES
Author notes
The authors are not recipients of research scholarships



