-
PDF
- Split View
-
Views
-
Cite
Cite
Tsuyoshi Hata, Nobuyasu Hayashi, Shoichiro Urabe, Koji Hayashi, Tomo Nakagawa, Toshiya Michiura, Kazuo Yamabe, Reduced-port laparoscopic appendectomy for acute appendicitis in pregnancy, Journal of Surgical Case Reports, Volume 2020, Issue 6, June 2020, rjaa097, https://doi.org/10.1093/jscr/rjaa097
Close - Share Icon Share
Abstract
Current guidelines indicate that laparoscopic appendectomies are safe for pregnant patients with acute appendicitis. Recently, single- and reduced-port laparoscopic surgeries have gained popularity for nonpregnant patients, because they minimize abdominal wall trauma. Here, we describe a reduced-port laparoscopic appendectomy (RPLA) in a 31-year-old pregnant female performed at 27 weeks gestational age. Preoperative abdominal ultrasonography and computed tomography imaging showed an inflamed, swollen appendix and blood test results showed elevations in the white blood cell count and the C-reactive protein level. Accordingly, acute appendicitis was diagnosed. A surgical incision was performed at the umbilicus with an EZ-access device; an additional 5-mm trocar was placed at the right lower quadrant. Recovery was uneventful. The patient was discharged 8 days postoperatively. A vaginal delivery was achieved at term. The RPLA was a good surgical option for minimizing surgical invasiveness, without increasing the technical difficulty, in conditions where the uterus and fetus are growing.
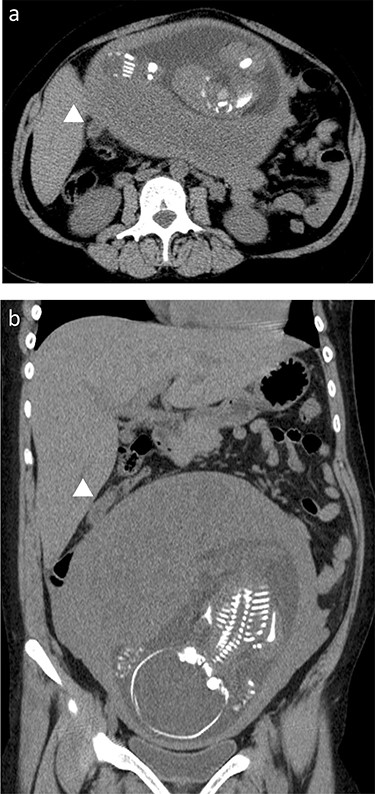
Preoperative CT scan; the swollen appendix (arrows) was translocated to the upper abdomen, and it can be observed underneath the liver, near the gallbladder; (a) axial view, (b) coronal view.
INTRODUCTION
In the technical development of laparoscopic surgery, the introduction of single- and reduced-port surgery, including double-incision laparoscopic surgery and needlescopic surgery, has minimized the number and total size of abdominal wall traumas. Accordingly, these techniques are widely accepted and practiced for appendectomies in patients with acute appendicitis [1–4]. For pregnant women, recent evidence has shown that laparoscopic surgery could be performed safely in any trimester without increasing risk to the mother or fetus [5]. However, no previous studies have investigated the reduced-port laparoscopic appendectomy (RPLA) for acute appendicitis during pregnancy. In the present case study, we describe the RPLA performed in a pregnant woman with appendicitis.
CASE REPORT
A 31-year-old pregnant female at 27 weeks gestational age visited our hospital with symptoms of acute epigastralgia, which had moved down to the right lower intestinal quadrant, and vomiting. She was gravida 8 and para 7, with no history of abdominal surgery. The blood exam showed an elevated white blood cell count (17 200/μl) and a high C-reactive protein level (2.01 mg/dl). The appendix could be detected with abdominal ultrasonography; it was inflamed and swollen to a length of 12 mm. A computed tomography (CT) scan was performed to confirm the degree of appendix inflammation and its location, showing the dirty fat sign and a swollen appendix located underneath the liver, close to the gallbladder fundus (Fig. 1a and b). The patient was clinically diagnosed with acute appendicitis. An emergency laparoscopic appendectomy was performed with the RPLA approach.
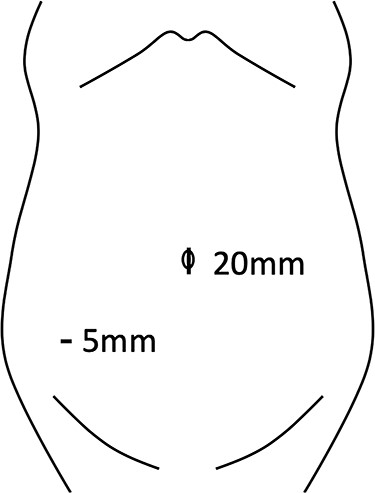
A lap protector with an EZ-access device and two 5-mm trocars were attached to the 20-mm umbilicus incision with the Hasson technique. CO2 insufflation was maintained at 10 mmHg. An additional 5-mm trocar was inserted in the right lower quadrant (Fig. 2). To gain a good field of view, the operation table was tilted to the left (Fig. 3a). The inflamed appendix was covered with omental adhesion in the space between the liver and the extended uterus (Fig. 3b). The appendix was dissected with laparoscopic coagulating shears and the pus was drained and collected (Fig. 3c). A tocolytic agent was administered by the obstetrician to prevent preterm delivery.
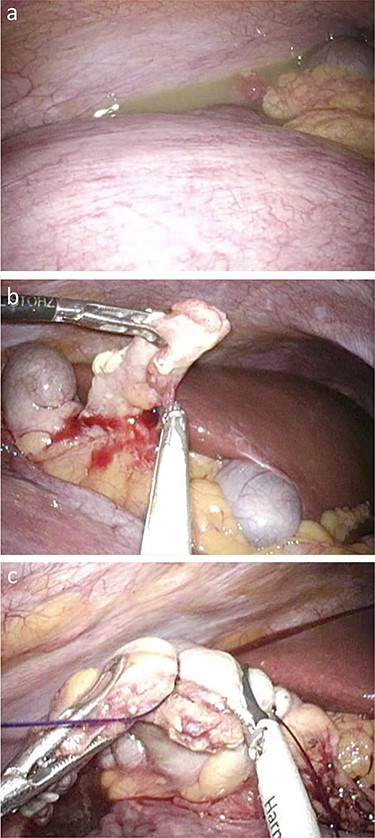
Operative findings; (a) the growing uterus with fetus, which pushed up the ileocecum under the liver, and the drain for pus collection; (b) dissection of the mesoappendix with laparoscopic coagulating shears; (c) dissection of the appendix after ligating the appendix base.

Operative scar 6 weeks after surgery (at 33 weeks gestational age).
The patient was allowed to drink clear fluids on the first postoperative day (POD), and solid food intake was started on POD3. Antibiotics were administered until POD4. The patient was discharged on POD8 without any postoperative complications (Fig. 4). A vaginal delivery was achieved at term.
DISCUSSION
The incidence of acute appendicitis during pregnancy was reported to be 0.05–0.13%, and it is the most common nonobstetric emergency [6]. The perforation rate of appendicitis is 14–43% in pregnant women, which is higher than the rate for nonpregnant women [7]. The incidence of fetal loss is 36% in women with a perforated appendicitis, and only 1.5% in women with nonperforated appendicitis [8]. This finding emphasized the critical need of early intervention in acute appendicitis during pregnancy. In 2017, the Society of American Gastrointestinal and Endoscopic Surgeons (SAGES) updated the guidelines for the use of laparoscopy during pregnancy. They stated that nonoperative management of uncomplicated appendicitis was not recommended, due to the high risk of peritonitis, fetal demise, shock and venous thromboembolism, compared to operative management [5]. However, an appendectomy during pregnancy runs the risk of preterm delivery, due to the difficulty in gaining a field of view, which leads to contact and compression of the uterus, when attempting to locate the appendix [6]. To overcome these issues, surgeons are beginning to accept the laparoscopic appendectomy as a practical approach in pregnancy [6]. A previous study, in 2007, demonstrated that laparoscopic appendectomy led to an unfavorable fetal outcome compared to open surgery [9]. However, currently, there is insufficient evidence to conclude that a laparoscopic appendectomy runs a higher risk of fatal loss than open surgery [5]. The SAGES guidelines indicate that laparoscopic appendectomy is the preferred choice for treating pregnant patients with acute appendicitis; moreover, laparoscopy is accepted for other diseases, including cholecystitis [5].
To reduce invasiveness even further in laparoscopic surgery, the single-incision and the reduced-port laparoscopic approaches were recently introduced into the field of abdominal surgery [10]. Prospective randomized studies and meta-analyses compared the single-incision (SILA) and conventional (CLA) laparoscopic appendectomies. Those groups showed similar perioperative outcomes, including the length of hospital stay and postoperative complications. In addition, the SILA group showed faster recovery than the CLA group [1]. Currently, the SILA has become a common, popular option for treating appendicitis. On the other hand, several studies showed that the SILA required advanced laparoscopic skills and tended to require slightly longer operating times, compared to the CLA [1–3].
Reduced-port surgery employs an umbilical-port approach, with one additional trocar. It can be regarded as a technical bridge between the SILA and CLA. Previous studies have shown the feasibility of the RPLA [2, 4]. They showed that the RPLA did not increase the surgical difficulty and that, similar to CLA, the RPLA approach facilitated instrument triangulation and provided better hand–eye and hand–hand coordination, compared to the SILA approach. In the current case study, the small umbilicus incision was made with an additional 5-mm incision in the right lower quadrant at the abdominal wall of the gravid patient. Although a SILA approach at the umbilical site might have been less invasive, in terms of the number of incisions, it strongly restricted access to the appendix, in the presence of the growing uterus and fetus, particularly in the third trimester. Indeed, the potentially frequent contact and compression of the uterus with the forceps could increase the risk of a preterm delivery. Under these conditions, an RPLA provided access for an additional pair of forceps through the right lower quadrant. Thus, the operator could use both hands to maneuver more safely and avoid direct contact with the pregnant uterus.
This case study reported our experience of a successful RPLA in a pregnant female with acute appendicitis. We provided further evidence to establish the safety and feasibility of an RPLA during pregnancy.
Conflict of interest statement
None declared.
References
- pregnancy
- appendicitis
- computed tomography
- blood tests
- fetus
- gestational age
- laparoscopy
- leukocyte count
- preoperative care
- surgical procedures, operative
- umbilicus
- wounds and injuries
- c-reactive protein measurement
- diagnostic imaging
- guidelines
- uterus
- abdominal wall
- trocar
- vaginal delivery
- abdominal ultrasonography
- appendectomy, laparoscopic
- medical devices



