-
PDF
- Split View
-
Views
-
Cite
Cite
Zakaria Ramzi, Jordi Juanos Cabans, Harold Jennart, Terrible triad of the elbow with an ipsilateral Essex-Lopresti injury: case report, Journal of Surgical Case Reports, Volume 2020, Issue 6, June 2020, rjaa103, https://doi.org/10.1093/jscr/rjaa103
Close - Share Icon Share
Abstract
Terrible triad of the elbow and the Essex-Lopresti injury are both rare lesions with a historically poor clinical outcome. We present the case of a unique association of the two injuries with an elbow dislocation, radial and coronoid process fractures and a distal radioulnar joint dislocation due to an interosseous membrane rupture. The case was managed with closed reduction of the elbow dislocation and distal radioulnar joint followed by open reduction and repair of the damaged structures in the elbow and an unloading of the interosseous membrane. A high index of suspicion with a detailed examination of the elbow, forearm and wrist associated to a comprehensive imaging were mandatory for a complete diagnosis and an adequate treatment. Six months after the accident, the patient made a good recovery.
INTRODUCTION
The terrible triad of the elbow and the Essex-Lopresti are two rare injuries but their association is unique [1, 2]. The terrible triad refers to three combined lesions: elbow dislocation, radial head and coronoid fractures [2, 3]. When the radial head fracture is accompanied by an interosseous membrane lesion affecting the distal radioulnar joint (DRUJ), it is given the name Essex-Lopresti injury [4]. We report on the diagnostic and treatment challenge of this unique case.
CASE PRESENTATION
A 56-year-old male fell forward onto his forearm and elbow during a mountain walk. He reported immediate swelling and pain in his elbow and wrist. On examination, there was a deformity of his right elbow with pain in the ipsilateral wrist; there were no skin or distal neurovascular disorders. Initial lateral radiographs requested by the emergency doctor focused on the elbow and showed a posterior dislocation of the right elbow with a type II Mason radial head fracture with a small detached fragment <20%, associated to a proximal radioulnar joint (PRUJ) dislocation and a coronoid fracture type 2 according to the O’Driscoll classification with an anterior avulsion of an anteromedial coronoid small fragment (Fig. 1A). There was mild widening of the DRUJ with significant ulnar negative variance (Fig. 1B).

(A) X-ray of elbow profile shows the posterior elbow dislocation with a detached anterior fragment from the coronoid; (B) three-fourth X-ray of the forearm before the reduction demonstrates significant ulnar negative variance.
As emergency treatment, we realized a closed reduction of the elbow dislocation under general anaesthesia with X-ray control, the limb was stabilized in a posterior brachiopalmar splint. A computed tomography (CT) confirmed the stage 2 coronoid process fracture and a partial radial head fracture, the PRUJ dislocation was also demonstrated (Fig. 2). The DRUJ and PRUJ dislocations were suggestive of a complete disruption of the interosseous membrane. We managed a surgical treatment the second day of admission. A Kaplan approach was used to reduce the PRUJ dislocation, the annulate ligament was repaired and the radial head fracture was evaluated, as the detached fragment was <20% of the radial head circumference, no fixation was necessary. The lateral collateral ligament (LCL) and the common extensor muscle were repaired. The elbow testing objected a stable elbow from −30° of extension to complete flexion. According to that elbow stability status and the coronoid fracture stage, we decided a conservative treatment for the anteromedial coronoid fracture. Closed reduction of the DRUJ was achieved but it was instable, a fixation with a TightRope was used (Fig. 3). The stability was rechecked and upgrade of the stable range of motion (ROM) was assessed, the elbow was now stable from −20° extension to complete flexion. A sling was used for comfort for 2 weeks postoperatively with physiotherapy and ROM exercises initiated early.
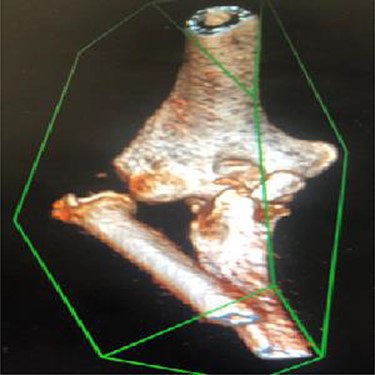
3D reconstruction CT scan of the elbow shows a radioulnar proximal dislocation with O’Driscoll type 2-2 anteromedial fracture.

Anteroposterior X-ray of the wrist showing the DRUJ reduction and the TightRope stabilization.
At 8 months of follow-up and 2 months of physiotherapy, the patient made a good recovery in regard to pain and mobility. Mobility of the right elbow was −20° for extension and 100° for flexion; the wrist mobility was respectively 60° and 20° of flexion and extension. The elbow was stable, and the grip strength was comparable to the contralateral side (Fig. 4A and B).

DISCUSSION
We present a particular case by the unique association of two rare injuries: a terrible triad of the elbow and an ipsilateral Essex-Lopresti entity. No similar case has been found in the literature review. The terrible triad includes a posterior dislocation of the elbow with radial head and coronoid fractures, concurrent ligament injuries are very common especially the LCL and medial collateral ligament (MCL), which can be the source of a definite instability [1, 2]. The Essex-Lopresti refers to an association of a radial head fracture dislocation, an interosseous membrane rupture and a DRUJ dislocation [3].
The elbow dislocation is a frequent and an easily diagnosed pattern, at the opposite of the DRUJ dislocation, which is often missed in the emergency department if an adequate physical exam with the appropriate radiographs is not carried out [3]. Distal arm pain should not simply be dismissed as referred pain [5]. Consequently, each time a radial head fracture associated or not to an elbow dislocation is diagnosed, an ipsilateral wrist examination is mandatory to diagnose an Essex-Lopresti injury; otherwise, chronic wrist symptoms can develop, such as pain and instability [4]. If plain radiographs are inconclusive or there is diagnostic uncertainty, further imaging with magnetic resonance imaging and CT are important [4].
The purpose of treatment in the terrible triad injury is to restore the congruency of the elbow joint, its stability and an optimal ROM. Surgical management is quite standardized according to Pugh et al. [6, 7]: (i) the humeroradial joint: LCL complex must be repaired in all cases eventually with the common extensor origin, radial head fractures are either treated functionally if minimally displaced, fixed, or if comminuted, replaced by an implant. Resection of radial head alone is contraindicated. (ii) Repair of the anterior column: by suture of the anterior capsule or fixation of coronoid process. (iii) The stability of the elbow is assessed; if still unstable, a hinged external fixator or repair of the MCL is discussed. The use of a hinged external protection is recommended as it allows quick articular mobilization [8]. (iv) Early elbow mobilization is started to avoid the stiffness. A study [9] has shown that coronoid fractures do not need to be fixed if there is stability in the ROM after repair of lateral structures. In case of instability, whatever the height of the fragment, fixation is indicated [5]. In our case, the testing showed a stable elbow, so we decided not to fix the coronoid fracture furthermore that it was a small anteromedial fragment stage 2 according to the O’Driscoll classification. The distal radioulnar dislocation should also be reduced by placing the forearm in maximum supination and stabilized either with a brachiopalmar splint, a percutaneous Kirschner wire, repairing the triangular ligament or the central band of the interosseous membrane [10]. We used a TightRope device to stabilize the DRUJ as this tool enables forearm good ROM at the beginning of physical therapy, and there is no need to remove the device.
Conflict of interest statement
None declared.
Funding
The authors declare there is no financial support from any organism.
Patient consent
Obtained.



